With transaminase elevated, can statins continue to use?
Sun Guolong from Ding Xiang Garden
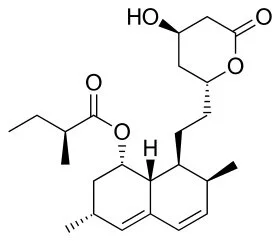
Statins, namely hydroxymethylglutaryl CoA (HMG-CoA) reductase inhibitors, By inhibiting the synthesis of cholesterol in the body, play the role of lipid regulation, but also stable atherosclerosis plaque, anti-inflammatory, improve the stability of vascular endothelial cells and other functions, clinical widely used in coronary heart disease, stroke and other diseases of secondary prevention.
But clinically, many patients with statins have elevated transaminase in the course of treatment, and some patients even develop drug-induced hepatitis. Can statins continue to be used after liver dysfunction? How should the indications and strategies of drug modification be defined
01. What are the characteristics of statin-induced transaminase elevation?
Related data show that all statins may cause elevated transaminase. In approximately 1-2% of all patients receiving statins, elevated liver enzyme levels were more than three times the upper limit of normal.
The increase of transaminase induced by statins occurred in a dose-dependent manner within 3 months after drug initiation, and the liver enzyme level decreased after drug cessation.
At present, most scholars believe that transaminase transient beyond the normal range is the result of organ adaptation to statins and cholesterol reduction, not a sign of liver damage.
02. Elevated transaminase occurs. How to adjust medication?
1. For asymptomatic patients with simple elevated transaminase (transaminases < 3 ULN), there is no need to adjust dosage or discontinue treatment;
2. If AST and / or ALT ≥ 3 ULN during the course of administration, the drug should be stopped or reduced, and liver function should be reviewed weekly until normal;
3. Patients with elevated transaminase accompanied by large liver, jaundice, elevated direct bilirubin or prolonged coagulation time should be considered for withdrawal;
4. Patients with mildly impaired liver function with nonalcoholic fatty liver (NAFLD), hepatitis B (HBV), and hepatitis C (HCV) and compensatory cirrhosis, It is safe to use statins. Liver function monitoring should be strengthened in patients with HBV and compensated cirrhosis.
5. Statins are prohibited in patients with active liver disease, decompensated cirrhosis and acute liver failure;
6. Rosuvastatin is hydrophilic, 90% of which is excreted through the kidney in its original form. It should be used in patients with liver dysfunction.
7. Atorvastatin, simvastatin and other mainly through the liver metabolism after clearance by bile, renal dysfunction should be used.
03. Or Alternative Medicine
1. Ezekimeb
As a cholesterol absorption inhibitor, ezetimibe is the second-line drug of choice when current statin intolerance or treatment with statins alone is substandard.
In clinical controlled studies with ezetimibe alone, the incidence of elevated transaminase (ALT / AST ≥ 3 ULN) was similar to that of placebo.
For patients with mild hepatic insufficiency (Child-Pugh score 5-6), there is no need to adjust the dosage. Ezetimibe is not recommended for patients with moderate to severe liver dysfunction.
2. Bile Acid Chelators
As basic anion exchange resin, it binds with bile acid in the small intestine to prevent its reabsorption, and promotes cholesterol synthesis of bile acids in the liver, thereby increasing the activity of liver LDL-C receptor and removing LDL-c from plasma.
Common adverse reactions include gastrointestinal discomfort, constipation and affecting the absorption of certain drugs. Absolute contraindications for such drugs are complete biliary atresia, abnormal beta-lipoproteinemia, and serum TG > 4.5 mmol/L (400 mg/dL).
3. PCSK9 inhibitors
PCSK9 is a secretory serine protease synthesized by the liver, which binds to and degrades LDL receptors, thereby reducing the removal of LDL-C from serum by HDL receptors. By inhibiting PCSK9, LDL receptor degradation can be prevented and LDL-C clearance can be promoted.
The results showed that PCSK9 inhibitors, either alone or in combination with statins, significantly reduced serum LDL-C levels and improved other lipid indicators.
Preliminary clinical findings suggest that the drug reduces LDL-C by 40 to 70 percent and reduces cardiovascular events. No serious or life-threatening adverse reactions have been reported so far.