Does Dostarlimab Really Cure Colorectal Cancer 100%?
In recent months, the miraculous efficacy of dostarlimab (Jemperli) has garnered widespread attention online, with some users claiming that the drug has achieved "100% cure for colorectal cancer" in the U.S.
Justin Lee 2025-01-22
In recent months, the miraculous efficacy of dostarlimab (Jemperli) has garnered widespread attention online, with some users claiming that the drug has achieved "cure for colorectal cancer" in the U.S. One user, identified as @Lawrenc09874431, even asserted that every patient taking this medication has been cured of colorectal cancer without the need for chemotherapy or surgery. Faced with such exciting claims, a friend reached out to me via WeChat for help. However, we cannot overlook the need for a thoughtful examination of such impressive yet unverified statements.
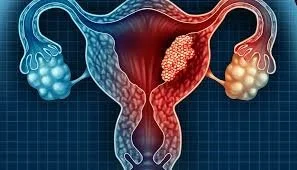
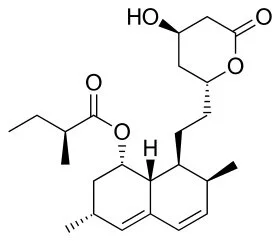
First, it is important to clarify that dostarlimab is neither a chemotherapy nor a radiotherapy drug; it is an antibody therapy, which we can generally understand as an immunotherapy drug. Initially developed by pharmaceutical company GSK, dostarlimab is a monoclonal antibody originally used for treating endometrial cancer, marketed as Jemperli. GSK has even established a dedicated website (jemperli.com), where many FAQs focus on endometrial cancer. As research progressed, scientists gradually discovered the drug's potential in treating other cancer types, particularly in certain gastrointestinal tumors, leading to recommendations for dostarlimab in treating colorectal cancer associated with DNA mismatch repair deficiency (MMR-D). This gradual process highlights the importance of continuously exploring and discovering new indications in pharmaceutical research.
It's worth emphasizing that clinical cases show a 100% efficacy and improvement rate of dostarlimab in specific colorectal cancer patients, but this situation is limited to certain individuals. In reality, dostarlimab targets patients with MMR-D colorectal cancer. In these patients, the drug effectively combats cancer cells by blocking the PD-1 pathway and activating the immune system. The success of this treatment strategy reflects the significance of personalized medicine. Therefore, to thoroughly understand the targeted use of this drug, one must grasp two technical terms: DNA mismatch repair and PD-1.
What is DNA mismatch repair (MMR-D)?
Simply put, DNA repair refers to the cellular response to DNA damage, which can restore the original structure of DNA and re-enable its functions. Cells can have different repair responses to various types of DNA damage. In mammalian cells, four relatively well-established DNA repair pathways have been identified, one of which is called DNA mismatch repair (MMR). The MMR system is a mechanism within cells designed to fix errors that occur during DNA replication. When this mechanism is defective, the genomic stability of the cell is compromised, leading to cancer. Tumor cells in MMR-D patients typically exhibit a high mutational burden, making them more recognizable and vulnerable to immune system attacks. Dostarlimab enhances immune function by participating in this process, potentially leading to significant improvements for some patients after treatment.
What is PD-1?
PD-1, or programmed death-1, is related to programmed cell death and apoptosis, referring to the orderly death of cells under genetic control to maintain environmental stability. Unlike cell necrosis, apoptosis is an active process involving a series of gene activations, expressions, and regulatory actions—it is not a pathological phenomenon but rather an adaptive death process for better environmental adaptation. PD-1 is an inhibitory immune checkpoint protein commonly expressed in T cells. Its primary function is to reduce immune responses and prevent autoimmune diseases. However, this mechanism is exploited by cancer cells in the tumor microenvironment to inhibit immune attacks. By blocking PD-1, dostarlimab lifts this suppression, allowing the patient's immune system to recognize and attack tumor cells again. Therefore, dostarlimab can have more pronounced therapeutic effects for MMR-D colorectal cancer patients.
In conclusion, dostarlimab indeed demonstrates powerful anticancer efficacy in certain populations, particularly in colorectal cancer patients with DNA mismatch repair deficiencies. However, this does not mean it can universally cure all late-stage colorectal cancer patients. Effective treatment requires precise patient selection; only individuals confirmed as MMR-D through current FDA-approved testing standards can receive effective treatment. Thus, patients should follow professional medical advice and make scientific and reasonable treatment choices to achieve optimal results. While dostarlimab is promising, it must be approached with caution and not seen as a panacea for the pursuit of a "cure."
Duesberg on AIDS
Today is World AIDS Day, and on this special day, we have to recall the denial and challenge of AIDS paradigm medical theory by a world-renowned molecular biology professor.
Justi Lee
Today is World AIDS Day, and on this special day, we have to recall the denial and challenge of AIDS paradigm medical theory by a world-renowned molecular biology professor.
Peter Duesberg, a molecular biologist and professor at the University of California, Berkeley, garnered significant attention in the 1980s and 1990s for his controversial stance on AIDS. Duesberg's assertions fundamentally challenge the prevailing view that the human immunodeficiency virus (HIV) is the primary cause of acquired immunodeficiency syndrome (AIDS). His arguments ignited heated debates and polarized opinions in both the scientific community and the public. Through the lens of the "5 Basic Objections" framework, this essay will explore Duesberg's critiques of the HIV/AIDS paradigm, the scientific responses to his claims, and the broader implications of his position.
Objection 1: Lack of Evidence Linking HIV to AIDS
Duesberg’s primary assertion is that there is insufficient evidence to conclusively link HIV to the development of AIDS. He argues that the correlation observed between HIV positivity and the onset of AIDS-related illnesses does not imply causation. Duesberg posits that AIDS may be the result of a combination of factors, including drug use, malnutrition, and exposure to various pathogens. He contends that epidemiological data supporting HIV as the causative agent is flawed and calls for a reevaluation of the evidence.
Counter-Argument
The majority of the scientific community, however, counters this claim with robust evidence supporting the HIV-AIDS link. Large-scale cohort studies and clinical research consistently demonstrate that HIV infection significantly increases the risk of developing AIDS. Numerous peer-reviewed studies have documented the progression from HIV to AIDS, illustrating the natural history of the disease. Furthermore, the successful implementation of antiretroviral therapy (ART) has shown a remarkable decline in AIDS-related morbidity and mortality among HIV-positive individuals, further substantiating the role of HIV as a causative agent.
Objection 2: Advocacy for Non-HIV Related Causes
Duesberg’s theory proposes that factors such as lifestyle choices, particularly drug use and poor nutrition, may be the primary contributors to AIDS. He argues that the immune system's deterioration is linked to these external influences rather than an infectious process initiated by HIV. This position points to the need for alternative explanations and solutions to combat AIDS.
Counter-Argument
Critics argue that by diverting attention away from HIV as the definitive cause of AIDS, Duesberg undermines public health efforts aimed at HIV prevention and treatment. The scientific community emphasizes the multifactorial nature of health, asserting that while social determinants and lifestyle factors undoubtedly play a role in health outcomes, this does not diminish the role of HIV as a critical factor in AIDS pathology. The integration of comprehensive care models that address both the infectious nature of HIV and the broader social influences is essential in tackling AIDS effectively.
Objection 3: Misinterpretation of Scientific Studies
Duesberg maintains that the scientific literature surrounding HIV and AIDS is plagued by bias and misinterpretation. He claims that researchers have failed to address alternative explanations for the data related to HIV infections and that this systematic bias obscures the truth about AIDS's real causes.
Counter-Argument
The response from the scientific community highlights the rigor of peer review and the reproducibility of findings in HIV research. Numerous studies, including those conducted under various methodological frameworks, consistently support the conclusions that identify HIV as the causative agent of AIDS. Moreover, the field of HIV/AIDS research is characterized by transparent and open discussions, which have undergone continuous scrutiny and validation, countering claims of biased interpretations.
Objection 4: Critique of Antiretroviral Therapy
Duesberg has been vocally critical of antiretroviral therapy (ART), equating it to a harmful intervention rather than a beneficial treatment for HIV-positive individuals. He raises concerns about the potential toxicity and side effects of these medications, asserting that they may contribute to immune system deterioration rather than bolster it.
Counter-Argument
Contrary to Duesberg's assertions, ART has been heralded as a breakthrough in the management of HIV/AIDS. Clinical trials illustrate that when taken as directed, ART can suppress viral load to undetectable levels, significantly reducing the risk of AIDS-related complications and transmission of the virus. The constructive critique of ART is essential in refining treatment protocols; however, dismissing the therapy outright undermines the evidence of its efficacy.
Objection 5: Ethical and Social Implications
Duesberg’s views have raised ethical concerns, particularly regarding how they influence public perception and policy surrounding HIV/AIDS. By propagating skepticism about HIV as a cause of AIDS, there is a potential risk of contributing to stigma against HIV-positive individuals and undermining public health initiatives.
Counter-Argument
The ethical obligation of the scientific community is to communicate transparently and accurately about health risks. Ensuring the widespread understanding of HIV as a determinant of AIDS is crucial not only for the health of individuals but also for the advancement of public health strategies aimed at combating the epidemic. The consolidation of scientific evidence reinforces the need for clear messaging that underscores the significance of prevention and treatment methods.
Conclusion
While Peter Duesberg's views on AIDS have sparked important discussions, the overwhelming body of scientific evidence supports the conclusion that HIV is the primary causative agent of AIDS. The complexities of the disease necessitate a multifaceted approach to treatment and prevention, yet the fundamental role of HIV cannot be disputed. It is imperative for the scientific community to uphold rigorous research standards and address conspiracy theories and misinformation that could potentially harm public health efforts in combating this devastating epidemic.
(It is worth noting that the University of Berkeley conducted a survey on his academic misconduct in 2009, but found that he was not responsible because the university believed that he had the right to publish those articles and did not judge the content of the study itself. In addition, I found that he co-published a paper with others in 2018. However, since 2010, the number of his research results seems to have decreased significantly. Considering that he is now 86 years old, this challenging academic insight on AIDS may no longer be succeeded under the suppression of paradigm science.)
Medical Points of View From PhD Jia
In general, leaders with such high risk should be aware of medical conditions, especially those at risk or hidden danger of heart disease. 一般来说,具有如此高风险的领导者应该注意健康状况,特别是那些有心脏病风险或隐患的人。
Hello! Everyone:
In general, leaders with such high risk should be aware of medical conditions, especially those at risk or hidden danger of heart disease.
You should live near a location with good medical conditions or convenient first aid, because there are many options in Shanghai, such as the West Suburb Hotel or the Hongqiao Reception Hotel, which is far better than the East Suburb Hotel.
Second, there are better hospitals in Puxi, just like the Zhongshan Hospital mentioned by Maoli just now. My teacher, Mr. Tang, is in Zhongshan Hospital. Zhongshan Hospital has two specialties, namely the liver department and the cardiovascular department, which rank first in China. Where are we going to stay when we become old?,I have always adhered to such a point of view, in the environment of China, it is not in the beautiful mountains and rivers. Therefore, I summarize this point to make a little reminding, just like children going to school, when they are young, their parents usually choose school districts to stay.Because China's medical resources are highly unbalanced, aged people should be living near the hospital with good medical conditions, I think this is very, very important.
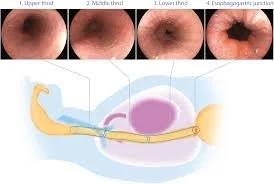
I mentioned about the physical examination the day before yesterday, and I already talked about the imaging examination, including the magnetic resonance of the head, the CT of the chest, and the B-ultrasound of the abdomen. Including the thyroid, as well as pelvic cavity, these can be checked with B-ultrasound, then there is another important reminding about the examination is the gastrointestinal tract. This is very important, if you have never seen a doctor for a colonoscopy, then I recommend scheduling a colonoscopy as soon as possible. If it is examined and there is no inflammatory lesion, that is, the inflammation is limited to ordinary inflammation, such as chronic non-atrophic gastritis, or general inflammation of the intestine, then in this case, once every two to three years can be OK.
But in some cases, we will have some positive display, such as chronic atrophic gastritis, or ulcers, or polyps, how to deal with these cases? Special emphasis is on multiple polyps, multiple intestinal polyps or stomach polyps, when such polyps are found, the doctor will remove them under the microscope, and will do pathology, which is generally more benign. There are also malignant, there are many kinds of classification, this does not expand to say, then there are a small number of polyps, it is itself malignant. These conditions may require a colonoscopy followed by surgery to remove a section of the intestine, or a major gastrectomy. However, benign polyps, especially multiple polyps, are likely to become cancerous within two to three years, so we know that gastroenteroscopy is very important, if it is multiple polyps, In this case, the period of gastroenteroscopy will be shortened by one year to one and a half years, if it relapses, after two to three years, the chance of cancer is very large.
Of course, as long as it is found to be early, I said that day for early malignant tumor, one only needs to do a small operation, and then radiotherapy and chemotherapy are not necessary. The prognosis is no different from that of normal people, and the duration of life is not affected.
Inflammation, especially autoimmune inflammation, such as intestinal Crohn's disease, or ulcerative colitis, which is increasingly common in China. In fact, the incidence rate in China has always been not low, just because we have confused this inflammation with other inflammation in the past, and then there is the lack of some basic examinations in terms of examination methods. The treatment of such diseases is generally immune agents or hormone methods to treat, the effect is limited, so this kind of inflammatory disease should be paid attention to early. Because when you happen early, it is controllable, and if it spreads down, it is more troublesome.
This type of disease usually manifests as gastrointestinal discomfort, long-term, chronic, recurring discomfort, such as abdominal soiling, repeated diarrhea. Like blood in the stool. Of course, these are not specific symptoms, because hematochezia may be a tumor, there may be hemorrhoids, there may be acute bleeding of the gastrointestinal tract, etc., this is more complicated, that is, there are some abnormalities to be highly concerned about.
Long-term and repeated inflammation, most of the results are tumors, so we should pay attention to inflammation, so for example, some inflammation in our mouth, and this digestive tract, just mentioned gastrointestinal inflammation, and female genital tract inflammation, and male urethra ah, and birthmark inflammation.
The main way to avoid and reduce inflammation is to avoid contact with or eat things that stimulate inflammation, such as polluting substances, special diets, such as eating too many peppers, too much alcohol, and cigarettes, etc., which are common things that everyone knows, to avoid exposure as much as possible, and radiation, heavy metal intake, and so on.
So if there is inflammation, then the physical examination can detect it and observe the progression of its malignancy, if it has an early invasive change. The lesions can be removed, and in that case, serious adverse consequences can be prevented.
Let me talk about some small effective methods, for example, many people suffer from chronic pharyngitis, which is indeed difficult to treat clinically. However, in my personal experience, I have cured many people with one method, and it is effective in a very short time, so this is recommended to everyone, because the general physique of Chinese people is similar, the use of western drugs and antibiotics, as well as local spray, hormones, these are effective, but no longer effective.
The medicine I am talking about is a Chinese patent medicine that can be taken orally, called Gui Fu Di Huang Pill. If you want to read the instructions, it does not write what is effective for inflammation, it is mainly the treatment of kidney deficiency, Yin deficiency, and weak fire.
The other is rhinitis, my experience, the simple and effective method, but needing to insist on a period of time, is to wash nasal cavity with saline water, now there is a special nasal wash, it is easy to buy online, very cheap, and then once or twice a day, it is allergic rhinitis, Or some other infectious rhinitis and so on. My experience is very effective ah, also I recommend to everyone. in fact, some diseases do not have to use drugs method to treat.
There is the physical examination, genetic testing is actually unnecessary, genetic testing is currently the most useful thing actually after the illness, for us. When you get sick, some of its drugs, like targeted drug therapies, need to find the mutant strain of this gene, and then you have to do genetic testing. Other scenarios, such as saying that the high expression of a certain gene means a high risk of certain diseases, this logic exists, he just said that there is this risk, but if you do not happen, to worry about this matter is not necessarily a good thing, so we only need to pay enough attention to routine physical examination and use effective ways and methods to detect. You can detect what should be detected, there is no need to use that sounds lofty and actually does not make much sense to predict. So this genetic testing is a misunderstanding, in addition, is often after the physical examination to do some intervention, in terms of health intervention, the more expensive is mainly stem cells, then this stem cell is also unnecessary, now there are two meaningful points in the work of stem cells, the first is cell storage, if we worry about the future. What's going to happen, which is actually now or before now, is that we're going to store some bone marrow stem cells, or some other healthy cells from certain parts of the body, and then we're going to use them in the future, and what they're going to do, to be honest, is they're going to use them in the future, and that's the first point, and the second point is that individual diseases, It's treatable with stem cells, and it's basically limited to leukemia. This is a blood disease, including MDS and so on, will not expand to say. So, in general, if you need beauty, or life extension, you use stem cells, which are unreliable, and a lot of them are deceptive. What about the physical examination, I think it is about this, but each person, each individual, his physical condition is different, including what has happened, or potential, the future may happen. They are also different, so if you have any personal questions, you can ask me individually, and I will try to answer them. thank you!
6-month consequences of COVID-19 in patients discharged from hospital: a cohort study
Lancet
Introduction
As of Jan 4, 2021, the global pandemic of COVID-19—an emerging infectious disease caused by SARS-CoV-2—has resulted in more than 83 million confirmed cases with more than 1·8 million deaths. The epidemiological and clinical characteristics, pathogenesis, and complications of patients with COVID-19 at acute phase have been explicitly described,but the long-term consequences of the illness remain largely unclear.
Long-term follow-up studies on persistent symptoms, and lung function, physical, and psychological problems of discharged patients are urgently required.
Only a few studies with small sample sizes have been published, with the longest follow-up duration being 3 months following discharge from hospital.
Some persisting symptoms such as fatigue and dyspnoea,impaired pulmonary function and chest image abnormalities were reported in patients following hospital discharge, but the full spectrum of post-discharge characteristics is still unknown. Furthermore, no studies have yet reported the extra-pulmonary organ manifestations that could persist after damage in acute stage or are newly onset after discharge.
We aimed to describe the long-term consequences of COVID-19 in patients after hospital discharge and identify the potential risk factors, including disease severity, associated with these consequences.
Background
The long-term health consequences of COVID-19 remain largely unclear. The aim of this study was to describe the long-term health consequences of patients with COVID-19 who have been discharged from hospital and investigate the associated risk factors, in particular disease severity.
Findings
At 6 months after acute infection, COVID-19 survivors were mainly troubled with fatigue or muscle weakness, sleep difficulties, and anxiety or depression. Patients who were more severely ill during their hospital stay had more severe impaired pulmonary diffusion capacities and abnormal chest imaging manifestations, and are the main target population for intervention of long-term recovery.
How ChatGPT Helps Medical Treatment?
ChatGPT 是一种人工智能技术,它使用自然语言处理来分析和理解人类对话。 ChatGPT 可以通过多种方式应用于医疗领域,例如改善患者体验、加强医疗咨询以及支持诊断和治疗过程。
Justin D. Lee
ChatGPT is an artificial intelligence technology that uses natural language processing to analyze and understand human conversation. ChatGPT can be useful in the field of medical treatment in various ways, such as improving patient experiences, enhancing medical consultation, and supporting the diagnosis and treatment process. Here are some of the ways ChatGPT helps medical treatment:
1. Improving Patient Experiences: ChatGPT can be utilized in medical centers and healthcare settings as a virtual assistant to improve patient experiences. Patients can converse with ChatGPT and obtain quick, personalized responses to their questions, which can help them feel more in control of their treatment and less overwhelmed by the medical process.
2. Enhancing Medical Consultation: ChatGPT can aid doctors and other medical professionals in their work by assisting in medical consultations. ChatGPT can be used to answer patient questions, provide relevant medical information, and suggest follow-up tests. This can help healthcare providers to be more efficient and effective in their work and allow them to focus on more complex cases.
3. Supporting the Diagnosis and Treatment Process: ChatGPT can be used to analyze data and generate insights that support the diagnosis and treatment process. By processing data from sources such as medical records, clinical databases, and medical literature, ChatGPT can help to identify patterns and trends that are critical to diagnosis and treatment. This can save valuable time in finding a diagnosis.
4. Providing Early Warning Signs: ChatGPT can track a patient's data over time and provide early warnings on any potential health risks to the patient or any changes in their health conditions. Such lead-up time can enable medical practitioners to provide early intervention and prevent extreme health issues.
Overall, ChatGPT has the potential to positively impact medical treatment by improving patient experiences, enhancing medical consultation, supporting the diagnosis and treatment process, and detecting potential early warning signs. However, it is important to acknowledge that AI technologies like ChatGPT are still developing and require extensive verification, validation, and training to be used in the healthcare industry.
Population ageing in China: crisis or opportunity?
The Lancet
Filial piety—respect for one's parents, elders, and ancestors—is a deep-rooted virtue in China. But rapid economic development, along with rising individualism and shrinking family sizes, has eroded the social status of older adults in China. This change is coinciding with a huge increase in the number of older people. Many countries face an increasingly ageing population, but China is now home to the largest population of older people in the world. In 2019, 254 million people in China were aged 60 years or older. By 2040, this number is expected to increase to 402 million, making up around 28% of the population. These changes have profound consequences for health in China, with a rising risk and burden of non-communicable diseases and a soaring demand on health and social care systems. How can China adapt?
The traditional care model of the younger generation caring for older people will not provide the solution. China's fertility rate has fallen continuously in the past four decades, despite the introduction of pro-natalist two-child and three-child policies. India will soon overtake China as the world's most populous country, and the Institute for Health Metrics and Evaluation predicts that China's population will fall by 48% from 2017 to 2100. Instead, as a new Commission published this week in The Lancetargues, embracing and enabling healthy ageing is key.
The Peking University–Lancet Commission on the path to healthy ageing in China takes an optimistic perspective, outlining how healthy ageing represents a huge opportunity for China. Led by one of the leading think tanks in China—the National School of Development of Peking University—in collaboration with international experts from a range of disciplines, it lays out a series of policies aimed at not simply addressing the country's population crisis, but rather unleashing the intellectual and vocational capacities of the older population and the whole of Chinese society.
To do so will require changes in how and where care is delivered. The health of the current older generation in China is often complex, and can involve a high prevalence of comorbidity and multimorbidity, with consistent health disparities between rural and urban areas, and between men and women. Hoping to address these challenges by simply expanding the number of geriatricians and nurses in large hospitals is both unrealistic and unfeasible. Instead, the authors call for a move from disease-centred care to person-centred care; care for older people should be primarily community and family based, rather than hospital based. Such a recalibration will entail a huge culture shift: many people in China go directly to hospitals when in need of health services, bypassing primary care.
The huge gap in long-term care services must also be filled. In an analysis published in The Lancet Public Health, Jinquan Gong and colleagues forecast that an extra 14·02 million older Chinese people will need long-term care by 2030. Therefore, the commissioners say, promoting the development of interdisciplinary primary health-care teams, integrated into the community, for older people is imperative, including the establishment of mobile health and online health services to improve access.
The need for change goes beyond the health system. The commissioners acknowledge that social and economic inequities are pervasive and dictate the health of older people in China. To ensure financial security for all, China should subsidise medical care and education for the poorest people, adopting a life-course approach to the social determinants of health, and narrow socioeconomic gaps (eg, between those living in urban and rural areas). For example, working class women retire 10 years earlier than men in China, resulting in substantially lower pensions and large gender inequalities. Raising the retirement age of women to that of men would help to reduce this disparity.
This is an ambitious set of recommendations, which apply across many sectors of Chinese society. They will not be fulfilled without strong political will. The importance of population ageing was recognised in the last month's National Congress of the Chinese Communist Party, where President Xi Jinping spoke of the construction of a healthy China, and the prioritisation of health. He vowed to actively respond to population ageing, develop the elderly care system, and ensure all older people in China can enjoy essential care and support. These are sensible priorities, given China's demographic trajectories. The Peking University–Lancet Commission brings together the best evidence and provides the clearest path to making them a reality. The result would be good not only for older people, but for the health of China as a whole.
Defending reproductive rights to promote healthy ageing
The Lancet Health Longevity
The landscape of reproductive rights for women in the USA was drastically altered on June 24, 2022, when the Supreme Court voted to overturn Roe v Wade and Planned Parenthood v Casey, thereby removing the constitutional right to abortion. The response was swift, with abortions expected to be banned in 26 states. Globally, 41% of women of childbearing age live in countries with restrictive abortion laws and, as a result, approximately 23 000 women die from unsafe abortions each year. Stripping women of reproductive rights therefore has immediate effects on their health and wellbeing, with unsafe pregnancies and dangerous self-managed abortions increasing the risk of maternal mortality and crippling mental health issues.
It is important to look beyond these immediate effects to understand the long-term impact of abortion bans on ageing outcomes in women. Research has shown that access to abortions results in higher educational attainment and higher labour force participation for women; a study assessing abortion legislation in 97 countries showed that access to abortion led to a decrease in fertility rates, which in turn increased labour force participation for women. As gendered social roles largely dictate that women shoulder the bulk of childcare responsibilities, the decision to have children must often be considered in the context of education or careers, and women are left juggling competing roles. Education and workforce participation have been shown to reduce the risk of multimorbidity, functional problems, and cognitive decline. For example, the ongoing cognitive stimulation afforded by education and employment aids in bolstering cognitive reserve, which in turn can mitigate the risk of Alzheimer's disease and related dementias. Thus, depriving women of reproductive choice and thereby access to education, careers, and economic empowerment is likely to have lifelong, devastating effects on women as they age.
Although women are still less likely than men to participate in higher education and employment and are more likely to assume unpaid or domestic labour roles, the past century has seen gendered roles challenged. The narrowing of the gender gap in access to these opportunities has resulted in a narrowed gap in ageing outcomes. A study assessed the effects of birth cohort and education level on cognitive ageing and showed that, while men in earlier birth cohorts and in the low education group performed better on a cognitive battery, women in later birth cohorts and in the high education group outperformed men. Similarly, another study that explored the effect of education and labour force participation on sex differences in functional limitations by birth cohort found that the higher prevalence of limitations in older women, compared with men, from early birth cohorts was attenuated when socioeconomic factors were accounted for, and was entirely eliminated in more recent birth cohorts. The findings of these studies show the crucial contribution of education and employment opportunities to gender differences in cognitive and physical health outcomes in later life, and signal targets for interventions to forge gender parity and thereby promote healthy ageing in women.
The 1973 Roe v Wade decision was monumental in granting American women the freedom to delay childrearing in the interest of pursuing education and careers, with cascading positive effects on health and wellbeing in older age. The Supreme Court's overturning of this decision has stripped millions of women of the human right to age in good health, therefore reversing years of progress to reduce gender disparities in healthy ageing. Although the decision only affects the USA, it has wider implications as it could set a precedent for other countries. Hopefully, its media prominence will guide attention to the importance of promoting reproductive rights globally to protect healthy ageing in women. This is particularly pertinent in regions that have restricted access to family planning services for women and that are experiencing rapid population ageing, primarily sub-Saharan Africa, northern Africa, and western Asia. Reproductive rights are basic human rights, and removing these not only endangers the immediate health of young women but also lays a precarious foundation for their health trajectories into later life. As we continue to live longer, it is important that we recognise that the lifelong health of women today and of generations to come is now severely jeopardised.
Ending child marriage: ensuring healthy futures for girls
The Lancet
One in five women are married before the age of 18 years. This fact has serious ramifications for health and wellbeing. Child marriage is associated with pregnancy at a young age, dangerous complications during pregnancy and childbirth, HIV acquisition, and intimate partner violence. Demographic changes mean that the number of adolescents is increasing and therefore more people will be at risk of child marriage. Disruption to education and a rise in poverty caused by the COVID-19 pandemic is estimated to put another 10 million girls at risk of child marriage over the next decade, in addition to the 100 million who were already projected to become child brides. Ending child marriage involves health, legislature, the economy, education, culture, and religion, making interventions difficult to coordinate. Harmful norms, including gender inequality and social, religious, and cultural practices, can be difficult to change. For the poorest families, who are struggling to survive, marrying off a child early might appear to be the only option. What, then, will it take to end child marriage globally?
First, is an appreciation that child marriage is a truly global issue. 12 million child marriages happen each year, largely in northwest central Africa, south Asia, and South America. 76% of girls in Niger, 59% in Bangladesh, and 36% in Brazil are married before the age of 18 years. But the idea that child marriage is a concern only in the global south is false. There were nearly 300 000 child marriages during 2000–18 in the USA, where child marriage for girls and boys remains legal in 44 states. In Germany, where child marriage has been illegal since 2017, 813 child marriages were reported in 2017–20.
144 countries have committed to the Sustainable Development Goals target 5.3, to end child marriage to achieve gender equality by 2030. However, essential reproductive health interventions, such as contraception and abortion services, remain illegal or hard to access in many countries, not least in the USA, where the US Supreme Court has rescinded a 50-year-old decision on the constitutional right to abortion. This hypocrisy will lead to more girls and adolescents in poverty, at risk of dying from unsafe abortions, and marrying or cohabiting under the age of 18 years—for some, marriage is the culturally acceptable response to an unintended pregnancy. Keeping child marriage laws in place is often a misguided paternalistic response to the effects of other anti-reproductive health laws that make girls more vulnerable in the first place.
Fortunately, the legal environment surrounding child marriage is not entirely bleak. According to UNICEF, child marriage is decreasing globally because of laws that have raised the marrying age to 18 years and investments in interventions; most progress in the past decade has been in south Asia, where a girl's risk of marrying in childhood has dropped from nearly 50% to less than 30%. In England and Wales, a bill was passed in April, 2022, to raise the marrying age from 16 years to 18 years in the hope of ending forced marriage, with fines and up to 7 years’ imprisonment for any adult facilitating such a marriage. However, punitive laws can lead to unintended consequences, including underground marriages and penalising minors, that might further marginalise families, especially those in poverty. Besides, legal prohibitions are only effective if they are enforced. Rights for children, particularly girls, and women are fragile. Civil society, human rights, and gender watchdog organisations must be supported to hold leaders accountable to rights-based legislation.
Ultimately, raising the legal age of marriage does not address the root causes of child marriage. There are other effective interventions. A 2021 systematic review for the UN found that the most effective interventions to reduce the prevalence of child marriage helped girls to remain in school through cash or in-kind transfers. Expanding labour market opportunities to ensure economic independence and fostering the development of livelihood skills remove the incentives that drive girls into marriage.
Every girl should be able to imagine a future for herself in which she has an education, economic potential, the right to choose when to marry, and the bodily autonomy to decide when and if to have a child. The alternative is a world in which girls are commodities for sexual exploitation and for procreation. Laws permitting child marriage need to change. But the effects will be minimal without investment in programmes that empower girls, change social norms in families and communities, and provide services to address the inequities across health, education, and economic security that cause child marriage to begin with.
Can Drinking Coffee Prolong Life and Reduce Heart Disease Risk? How much daily drinking is the best?
China Medical Tribune
In many people's eyes, coffee is not only a drink, but also a culture, a way of life. For many, coffee has become the "standard" of everyday life.
At home, it allows people to spend time in a room filled with fragrance and experience slow life; When tired, it is the "good medicine" for office workers to recharge; Leisure time, it is an integral part of friends gathering and socializing.
But, drink coffee also should pay attention to method, how to drink will be more healthy?
Multiple studies presented recently at the 71st Annual Meeting of the American College of Cardiology (ACC 2022) Scientific Sessions show thatDrinking coffee, especially two to three cups a day, has been linked not only to a reduced risk of heart disease and abnormal heart rate, but also to longer life expectancy.Moreover, these trends apply to people with or without cardiovascular disease
Researchers stress that,The largest analysis yet of coffee's potential role in heart disease and death confirmed no link between coffee and having or worsening heart disease, on the contrary may have a protective effect on the heart.
Peter M. Kistler, MD, a professor at the Alfred Hospital and the Baker Heart Institute in Melbourne, Australia, and a senior researcher on the study, said "The data suggest that instead of banning coffee every day, it should be part of a healthy diet for people with or without heart disease." He further stated that “We found that coffee has a neutral effect, which means it's not harmful, and it may be good for you.。”
The research team used sample data from UK Biobank, a large, prospective database containing health information on more than half a million people who were tracked for at least 10 years. The researchers looked at the relationship between different coffee intakes ranging from one to more than six cups a day and the development of arrhythmias, cardiovascular disease (including coronary artery disease, heart failure and stroke), all-cause or heart-disease-related death in the subjects. Participants were grouped according to their reported daily coffee consumption (based on questionnaires completed at enrollment), such as 0, < 1, 1, 2-3, 4-5, or > 5 cups / day.
Overall, the researchers found two results:
1) Coffee consumption did not have any adverse effects on the subjects.
2) Controlling for factors that will affect heart health and longevity, including exercise, alcohol consumption, smoking, diabetes and hypertension, significantly reduced the risk of cardiovascular disease in many cases.
Drinking two to three cups of coffee a day has the best health benefits
In the first study, the effects of habitual coffee consumption on cardiovascular disease, cardiac arrhythmia and mortality were studied. Researchers evaluated data on 382,535 subjects with no known heart disease to see if coffee drinking played a role in the development of heart disease or stroke over 10 years of follow-up tracking. The average age of the subjects was 57 and half of them were women. The study found that
In general,Drinking two to three cups of coffee a day has the greatest benefit, reducing the risk of coronary heart disease, heart failure, heart rhythm problems or death from any cause by 10 to 15 percent.
Those who drank a cup of coffee a day had the lowest risk of stroke or heart-related death.
The researchers did observe a U-shaped relationship between coffee intake and new heart rate problems. Because subjects who drank more or less coffee each day had smaller benefits
The second study explored the association between regular coffee intake and improved mortality from cardiovascular disease in 34,279 people with different cardiovascular diseases. The findings:
Subjects who drank two to three cups of coffee a day were less likely to die than those who didn't.
Importantly, drinking any amount of coffee did not increase the risk of heart rhythm problems, including atrial fibrillation or atrial flutter, which the researchers say are often of concern to clinicians.
Among the 24,111 subjects with arrhythmias included in the analysis, the study showed that drinking coffee was associated with a lower risk of death. For example, subjects with atrial fibrillation who drank a cup of coffee a day may have nearly 20 percent lower mortality than those who didn't drink coffee.
“Clinicians generally do not recommend that people who already have cardiovascular disease or cardiac arrhythmia continue to drink coffee, so they are often overcautious and will advise them to stop drinking coffee altogether, But our study shows that regular coffee intake is safe and may be part of a healthy diet for heart disease patients.
Although drinking two to three cups of coffee a day seems to be the most beneficial, the researchers suggest that people should not increase their coffee intake, especially if it makes them feel anxious or uncomfortable.
Dr Kistler said: “Coffee drinkers should feel reassured that they can continue to enjoy their coffee even if they have a heart condition. Coffee is the most common cognitive enhancer - it refreshes and sharpens the mind. "
So how do coffee beans benefit the heart?
Coffee is often equated with caffeine, but coffee beans actually contain more than 100 bioactive compounds. These substances can help reduce oxidative stress and inflammation, increase insulin sensitivity, boost metabolism, inhibit the absorption of fat in the gut and block receptors known to be involved in abnormal heart rhythms, Dr. Kistler said.
In a third study, the researchers explored the impact of different coffee types on cardiac arrhythmic events, cardiovascular disease and mortality. They looked at whether there were differences in the relationship between coffee and cardiovascular disease, depending on whether people drank instant or ground coffee, caffeinated or decaffeinated.
Again, the study found that whether they drank freshly ground or instant coffee,Drinking two to three cups a day is associated with the lowest risk of arrhythmia, blocked coronary arteries, stroke or heart failure.Mortality rates were lower for all coffee types.
Decaffeinated coffee does not work well to prevent arrhythmias, but does reduce the incidence of cardiovascular disease, with the exception of heart failure.
Dr Kistler stressed that the findings show that caffeinated coffee is more popular and that decaffeinated coffee has no cardiovascular benefits.
In the future, further medical evidence will be obtained through trials
The team noted that the studies had several important limitations: The researchers were unable to control for dietary factors that may contribute to cardiovascular disease; Unable to adjust intake of any creamer, milk or sugar; The participants were predominantly white, so more research is needed to determine whether the findings extend to other populations.
Although research shows that people's eating habits don't change much in adulthood or over time. However, these results should be validated in randomized trials.
5 Steps to Lose Weight and Keep It Off
https://www.heart.org
Learning to balance healthy eating and physical activity can help you lose weight more easily and keep it off.
Take it from people who have successfully maintained weight loss:
98% have modified their eating habits.
94% have increased their physical activity, especially walking.
Source: National Weight Control Registry
Set realistic goals.
Know where you are today so you know how to get where you want to be. Learn your Body Mass Index (BMI). Set yourself up for success with short-term goals, like “I will make lifestyle changes which will help me lose (and keep off) 3-5% of my body weight.” Short-term goals can seem more achievable and keep you on track toward your long-term goals.Understand how much and why you eat.
Use a food diary or tracking app to understand what, how much, and when you’re eating. Being mindful of your eating habits and aware of your roadblocks and excuses can help you get real about your goals.Manage portion sizes.
It’s easy to overeat when you’re served too much food. Smaller portions can help prevent eating too much. Learn the difference between a portion and a serving and how to keep portions reasonable.Make smart choices.
You don’t have to give up all your favorite foods. Learn to make smart food choices and simple substitutions instead. Discover healthy snacks and how fruits, vegetables, and whole grains help keep you fuller longer.Be physically active.
Physical activity is anything that gets your heart rate up, like walking. Aim for at least 150 minutes of moderate activity a week. Move more, with more intensity, and sit less.
Summary of The global burden of adolescent and young adult cancer in 2019
The Lancet
Background
In estimating the global burden of cancer, adolescents and young adults with cancer are often overlooked, despite being a distinct subgroup with unique epidemiology, clinical care needs, and societal impact. Comprehensive estimates of the global cancer burden in adolescents and young adults (aged 15–39 years) are lacking. To address this gap, we analysed results from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019, with a focus on the outcome of disability-adjusted life-years (DALYs), to inform global cancer control measures in adolescents and young adults.
Methods
Using the GBD 2019 methodology, international mortality data were collected from vital registration systems, verbal autopsies, and population-based cancer registry inputs modelled with mortality-to-incidence ratios (MIRs). Incidence was computed with mortality estimates and corresponding MIRs. Prevalence estimates were calculated using modelled survival and multiplied by disability weights to obtain years lived with disability (YLDs). Years of life lost (YLLs) were calculated as age-specific cancer deaths multiplied by the standard life expectancy at the age of death. The main outcome was DALYs (the sum of YLLs and YLDs). Estimates were presented globally and by Socio-demographic Index (SDI) quintiles (countries ranked and divided into five equal SDI groups), and all estimates were presented with corresponding 95% uncertainty intervals (UIs). For this analysis, we used the age range of 15–39 years to define adolescents and young adults.
Findings
There were 1.2 million (95% UI 1·11–1·28) incident cancer cases and 3960 (3700–4250) deaths due to cancer among people aged 15–39 years worldwide in 2019. The highest age-standardised incidence rates occurred in high SDI (59·6 [54·5–65·7] per 100 000 person-years) and high-middle SDI countries (53·2 [48·8–57·9] per 100 000 person-years), while the highest age-standardised mortality rates were in low-middle SDI (14·2 [12·9–15·6] per 100 000 person-years) and middle SDI (13·6 [12·6–14·8] per 100 000 person-years) countries. In 2019, adolescent and young adult cancers contributed 23·5 million (21·9–25·2) DALYs to the global burden of disease, of which 2·7% (1·9–3·6) came from YLDs and 97·3% (96·4–98·1) from YLLs. Cancer was the fourth leading cause of death and tenth leading cause of DALYs in adolescents and young adults globally.
Interpretation
Adolescent and young adult cancers contributed substantially to the overall adolescent and young adult disease burden globally in 2019. These results provide new insights into the distribution and magnitude of the adolescent and young adult cancer burden around the world. With notable differences observed across SDI settings, these estimates can inform global and country-level cancer control efforts.
NURSING AWARD PUTS UTA ‘AMONG THE BEST IN THE COUNTRY’
ELIZABETH COUCH
The National League for Nursing (NLN) has named The University of Texas at Arlington as a Center of Excellence for the University’s sustained efforts to advance the science of nursing education.
It is the fourth time in recent years that UTA’s College of Nursing and Health Innovation (CONHI) has received a Center of Excellence designation from the NLN. Comprising 40,000 nurse educators and 1,200 member institutions, it is considered the premier organization for nurse faculty and leaders in nursing education.
CONHI is the No. 1 producer of baccalaureate-degreed nurses in Texas and a leader in addressing state and nationwide shortages of registered nurses. The college practices innovative health care research with internationally renowned faculty members specializing in cardiovascular conditions, aging, esophageal cancer, osteoporosis, bone disease, patient safety, health disparities and more.
UTA Interim President Teik C. Lim said CONHI’s continued commitment to innovation and its array of accessible programs has made it the premier nursing program in Texas.
“This prestigious recognition reinforces UTA’s position as one of the finest academic centers for nurses in the nation,” Lim said. “Through innovative and accessible degree programs that attract thousands of the brightest nursing students from Texas and beyond, UTA’s College of Nursing and Health Innovation has become an established leader in the critical field of educating, training and improving our nation’s nursing workforce.”
UTA becomes one of just a small number of universities nationwide to earn the Center of Excellence designation across all three NLN categories for nursing education: Advancing the Science of Nursing Education; Enhancing Student Learning and Professional Development; and Promoting Pedagogical Expertise of Faculty.
“This latest NLN designation highlights our commitment to conducting nursing education- related scholarship and research to generate the new knowledge needed to continually advance excellence in nursing education,” said Elizabeth Merwin, CONHI dean. “These designations are evidence of our college’s investment in training the future of our profession. We are thankful for our faculty and staff, who work tirelessly to ensure our college provides a world-class learning environment for all of our students while being a leading center for nursing education instruction and research as well as health care research.”
Megan Rogers, associate chair for undergraduate nursing, said the pandemic has demonstrated that advancing the science of nursing education is crucial to producing a qualified workforce for a field with ever-growing demand. “This designation puts us among the best in the country,” Rogers said. “It is a testament to the University’s investment in our faculty and to our core belief that you can know nursing, but you must also know how to teach to achieve the student outcomes we need.”
Kathryn Daniel, associate dean for academic affairs in nursing, pointed out that NLN designations require peer review from a variety of nursing leaders, making them especially significant.
“Nursing leaders across the country recognize that UTA performs at the highest possible level in terms of educating future nurses and future nursing leaders,” Daniel said. “UTA’s diversity in faculty, who bring their experience in a multitude of settings and roles within nursing, bolsters our place as a leader in nursing education.
“Employers who hire our student graduates can vouch for them. I would encourage future students to ask employers from where they want graduates. I can almost guarantee you they’ll say UTA.”
Catering Industry Transformation Driven by Consumption Upgrade
Deloitte
China’s catering industry has been integrated during the 12th Five-Year Plan period while high-grade catering consumption has been pent up, dragging down the overall industry growth. With strong consumption upgrade in 2016, the first year of China’s 13th Five-Year Plan, public catering consumption has started to grow rapidly with more diversified service targets and demands. Technological advances have also reshaped the consumption via consumers’ decision-making processes and payments. Driven by complex and changing demands as well as advancements in technology, catering, one traditional service industry, has seen a new round of opportunities for transformation and upgrading. Stable consumption growth helps strengthen the long-term positive prospect of catering market and attract more capital and crossover competitors. Deloitte believes that China’s catering industry will reach to a new stage of diversified development and competition over the next few years. Key observations of this report are as follows:
Consumption upgrade leads a rapid recovery in catering. In the trend of consumption upgrade, public catering has become the pivotal force in boosting the industry growth, as consumers are more willing to dine out. Meanwhile, the rising next generation of consumers bring more diversified demands, creating scope for growth in different types of catering categories.
Chain catering enterprises drive the entire industry to scale up and develop effectively. In recent years, chain enterprises with efficient operation and rapid expansion are taking center stages. Based on the findings of studies on these enterprises, business format/ brand innovation, digital transformation, industry chain extension and capital market operation will be the major development directions. Such measures will facilitate the industry transformation and upgrade in terms of product, service, quality and efficiency. Although the concentration of China’s catering industry remains low with a lack of enterprises at ten-billion level, there is much development space for chain catering groups and the industry is expected to see further expansion and integration.
The rise and adoption of technology promote the digital transformation of catering industry. Technology adoption, represented by the Internet, provides new channels for catering enterprises to connect with consumers and strong support for enterprise management. And thereby digital transformation proves to be one key development direction for catering enterprises. The application of emerging technologies, including big data and Internet of Things, also helps drive up the operation and management of catering enterprises.
Catering industry is more active in capital market. Catering enterprises have gained increasing attention from capital market and started engaging more actively in the capital operation. The approved IPO application of Guangzhou Restaurant puts and end to the absence of catering enterprises listing in the A-share for years, expecting to open up a new door for A-sharing listing of catering enterprises. Smaller catering enterprises have listed in NEEQ to obtain attention and support from capital. PE/VC investment for catering enterprises has also increased constantly with a sizable percentage invested in enterprises in angel rounds, reflecting investors’ optimism for catering industry. 2
Policy guidelines shall not be overlooked: tax compliance and food safety have become the regulation focus in catering industry. As the impact of policy guidelines on the industry is a major systematic risk for its development, catering enterprises need to develop prior planning with full attention to compliance issues to be not affected. Recent policies indicate that food safety has become the regulation focus while supporting the healthy industry growth; and relevant laws and regulations have been improved, tightening restrictions on enterprises. Tax and other issues caused by VAT reform also require sustained attention. For successful listing, enterprises shall advert to compliance in various aspects in early stages and avoid being impacted by non-compliance on listing progress.
Can vitamin C lower uric acid? A collection of popular medication questions!
Dingxiang Garden
1. Can vitamin C lower uric acid?
Yes.
Relevant literature shows that "vitamin C can reduce uric acid." The mechanism of action is: Vitamin C antioxidant effect can expand into glomerular arteriole, increase renal blood flow, thus increase glomerular filtration rate; Competition for tubular reabsorption.
2. What medications can be used to treat obesity?
Ciprofloxacin (naltrexone) / bupropion, lorcaserin, phentamine / topiramate, orlistat, liraglutide.
Currently, The main drugs approved by the United States Food and Drug Administration (FDA) to treat obesity are ciprofloxacin (naltrexone) / bupropion, lorcaserin, phentermine / topiramate, orlistat, and liraglutide.
But orlistat is the only drug approved in China with an indication for treating obesity. Orlistat for the treatment of obese and overweight (BMI ≥ 24 kg / m2) adults aged 18 years and over[1]。
3. How to choose anti-osteoporosis drugs?
Sub-situation selection.
Oral medications such as alendronate should be preferred in patients with low to moderate fracture risk. In elderly patients with oral intolerance, poor compliance and high fracture risk, such as multiple vertebral fractures or hip fractures, injections such as zoledronic acid and teripratide may be considered; Estrogen or selective estrogen receptor modulator such as raloxifene may be considered in patients with only a high risk of vertebral fracture but not hip and non-vertebral fracture. Short-term use of calcitonin may be considered in patients with new fracture and pain[2]。
4. What is the optimal route of administration of dopamine?
Administration via central venous catheter.
Dopamine is preferably administered via central venous catheter to eliminate the risk of drug extravasation. In the absence of a central venous catheter, bulky veins should be used for intravenous (intravenous) or intravenous drip (intravenous drip), while preventing drug extravasation[3]。
5. What is the preferred fluid for acute pancreatitis rehydration?
Isotonic crystal liquid.
Extracellular solutions (Ringer's Lactate, etc.) may be associated with anti-inflammatory effects, but evidence based on randomised trials is insufficient to demonstrate that Rlinger's lactate is superior to normal saline. Artificial colloids such as hydroxyethyl starch (HES) are not recommended due to increased risk of organ failure[4-6]. While correcting blood potassium levels.
Mother-in-law said I hurt a family of three generations: a hepatitis B mother's two births
Dingxiang Garden
Infected
The liver is a "silent" organ, and liver tissue without sensory endings cannot report its pain. In most cases, hepatitis B does not rapidly attack.The virus lingers in people for a decade or two, and if not told, the infected person won't even realize they have hepatitis B.
Gu Xia was diagnosed at the age of 14.
In the late summer of 1999, Gu's brother's school conducted a large-scale screening for hepatitis B infection. After the results came out, the school called, the other tone solemn, informed his brother infected with hepatitis B virus, and suggested that the whole family "go to screening again."
Also diagnosed were two small children from the next village. Three families packed a car to the CDC in the county, and the results came out that night -Gu Xia and the mother of another child were confirmed to have hepatitis B virus.
"How did you get it? "This is the hepatitis B virus infected people will be aware of the results after the repeated exploration of a problem. Gu Xia is no exception.
There are two things she can relate to.
At the age of seven, Gu fell ill with yellow skin, yellow urine, fever, weakness and an aversion to oil - considered a sign of liver disease locally. In the early 1990s, few people in Gu Xia's village would go to the city to seek medical treatment. "Children, whether they have hepatitis or smallpox, are looking for barefoot doctors, folk remedies and home treatment. ”
Grandpa punted across the river, took Gu Xia to find a local old man, more than sixty years old, dark and rough skin, not much. Farming is his main business, the local spread, the old family spread for generations to cure liver disease folk prescription.
The other eyelid lift, looked at the girl's face, "liver disease is right," gave her "a lump of black medicine mud," home rub into broad beans big pills, two pills a day.
"Now that I think about it, some of the acute symptoms may have disappeared, but I didn't go to the hospital for a check-up. Hepatitis may have been there ever since. ”
There are also risks from sharing needles.
Gu Xia, who has been in poor health since childhood, is a frequent visitor to the doctor's home. There was an aluminum lunch box on the doctor's desk, with an alcohol lamp under it, and a limited number of needles sunk into the bottom of the box.
"When I have a cold, go for an injection. When you're done, pull the needle off and put it back in the lunch box. When it's hot, it's sterilized. Change one of several needles from inside to the child behind, then change another. ”
But for Gu Xia, the "iatrogenic infection virus" speculation is not the most frightening. What is frightening is that "you may become the source of infection." She has a secret and deep guilt that she "may have caused her brother and other children to contract hepatitis B."
The introspection or condemnation of morality caused by the virus is not unique to Gu. Hepatitis B infection is considered to be the fault of the infected person, just as alcoholics are prone to esophageal cancer and smokers to lung cancer.People speculated that hepatitis B patients must have "done something unhealthy" to "attract such punishment."
A "post-80s" girl once mentioned that after being told by her school that she was infected with hepatitis B virus, her parents' first reaction was to accuse her of "eating out."This misperception still exists today.
Although the WHO document states: "Hepatitis B virus is not transmitted by sharing utensils or cooking utensils with an infected person, breastfeeding, hugging, kissing, coughing or sneezing by an infected mother. ”
Yet for hepatitis B, the rumors never stop.
From the early years, when laws and regulations imposed an unwarranted occupational ban on hepatitis B carriers, to the public's fantasies about pollution caused by the term, HBV carriers have to carefully hide their identity.Accordingly, they are deprived of many choices by life.
At the age of 15, Gu Xia graduated from junior high school did not continue to study, she wanted to work in a factory, relatives opened the food factory, medical examination was brushed down. "How many paths can a man like me, who hasn't studied much, choose? Either into the factory, or catering, but both tragedy. ”
Gu Xia eventually entered the beauty salon industry, "is the lowest threshold of admission." She started with the front cashier, trying to avoid direct contact with customers.
Before 2018, she worked outside, as far as possible choose to live alone, "can not give others trouble."
Birth
"Can it be cured? ”
"There is no cure for this disease. The cure is spending money for nothing. No amount of money can be spent on it. We can't get rid of the root. ”
In the four years since her diagnosis, Gu Xia has not given up, and the above conversations have occurred many times between her doctors and her.
The family does not give up, asking around may be "completely cured" of the folk prescription.
The first prescription left a lasting mark on Gu Xia and his brother. Uncle pulled a few herbs from the ridge of the field, mashed them, soaked them with soju and applied them to the wrists of the siblings. "Men left and women right, apply morning and night, flow pus water, disease is fine. ”
The siblings did not make it through the night, suffering burns, blistering, yellow water on their wrists and "rolling around in bed in pain."
Twenty years later, Gu Xia still has scars on the inside of her wrist from that year's injury."Reach out, people ask, I said when I was a child hot. ”
Gu Xia's wrist is white after the scab wound
Having suffered, Gu Xia did not stop there. She has tasted bitter soup and swallowed meatballs made of pig bile and flour. The inspection data given by the hospital is not always what she wants, "or big Sanyang."
Unable to get the desired result, Gu gave up completely, did not go to the hospital, no longer treated, pretending to go back to before the diagnosis - when she had not lost her "normal" status. For her, it was "a way to survive."
But there was one problem she could never get around - marriage and childbirth.
When she was 20 years old, Gu Xia and her partner of two years were about to enter a marriage. She confessed to each other. After consulting with her parents, her boyfriend sent her a reply:
"Our family would rather have an ugly daughter-in-law than an unhealthy one."
"I was particularly hurt by his attitude and at that time I had thought about it for a long time and thought it (the confession) was wrong and should have kept it from me. ”
Three years later, Gu Xia with a secret into the first marriage, the other side did not mention the pre-marital examination, she also avoided.
In 2009, she and her husband "drift north" to work together, pregnant.
The secret is still not well hidden. When she was six months pregnant, her husband suffered motion sickness and vomiting on his way to work. The doctor diagnosed acute hepatitis B virus infection and asked her family to check it out.
"I can't hide it. In front of his family, the doctor took my results and said, "You're obviously not infected right now." ”
When the husband and his family knew, their faces changed. Originally in and out will accompany her mother-in-law, since then never asked Gu Xia's body.
Doctors advised her to undergo "mother-to-child blocking," the first time Gu had heard of the term.
"At that time, I was looking for the director of a hospital in Beijing, because there was no file in the hospital, Is the field again, the doctor does not receive, also does not give cure, gave a suggestion, 'pregnant 7, 8, 9 three months continuously play hepatitis B immunoglobulin'. "The blocking rate is about 98 percent," the doctor told Gu.
Zhang Qingying, chief physician of the Department of Obstetrics and Gynecology Hospital of Fudan University in Shanghai, has 30 years of clinical experience. In her memory, "Mothers with hepatitis B virus use hepatitis b immunoglobulin in the third trimester of pregnancy" has been vigorously promoted.
But "in recent years, more clinical studies have not proved that it can improve the rate of maternal and infant blocking," "it simply can not play a blocking role, no inhibition of the virus, no protective effect on children. Then I didn't have to. ”
All that has happened since has confirmed this statement. But for Gu at the time, it was a lifeline, carrying a 50% chance. So long as the children are healthy, I shall have something to say about the family, and my marriage shall be preserved. ”
She returned to Anhui and begged doctors at the county's maternal and child health care hospital to inject herself with hepatitis B immunoglobulin.
A few months later, the child was born in a private hospital.Medical staff treat Gu Xia, there is no "this is a chronic hepatitis B maternal" such awareness, still according to the routine operation.
Gu Xia's son was born less than 12 hours after being vaccinated against hepatitis B and hepatitis b immunoglobulin. The former had been added to the national category one vaccine in 2005, which is free of charge and compulsory for all newborns. And if the mother carries the hepatitis B virus, the child must also add a dose of hepatitis b immunoglobulin.
There was a ten-month interval between the birth of the child and confirmation of the infection. Every day Gu Xia lives in a struggle. "I am a contradiction. I want to explore what this disease can do." But scared and didn't want to know. I feel that if I hadn't been checked out, my life would have been different, and it wouldn't be as miserable as it is now, "
"Naturally I hope he is healthy, and I don't want him to taste it again for my sins. I am afraid to know if he has hepatitis B, but I have to be responsible for him. ”
Hospital examination results shattered all her expectations, her son is "small three yang." (Note: The success rate of blocking between mother and baby is mainly related to the timeliness of newborn vaccine injection and maternal viral load. The blocking rate of vaccine + immunoglobulin is about 96%. )
When the child was born, her mother forbade Gu Xia from being close to her son. She did not allow lactation and separated dishes and chopsticks. Gu Xia held her son teasing for a while, her mother-in-law came forward to take the child away. "All her actions are saying, 'You're sick, you stay away from the kids, stay away" from us.
After the results of his son's tests, "behavior" became "language."
"She used to shout, 'You have destroyed three generations of our family'. ”
Husband to talk to Gu Xia: "You are sick, The child is also sick, I treat the child to a large amount of money, in case one day you also need such a large sum of money. We are husband and wife, from the moral point of view I should treat you, but I can't afford it. ”
I knew then that if we weren't married you could leave me alone. ”
After that conversation, Gu Xia's marriage ended.
"I explained that the doctor said it was an extinct volcano and that all it needed was to push it down with medicine. How do you know I must need a large sum of money for treatment? But I don't believe you, and I think that's a quibble. ”
Anxiety about the risk of mother-to-child transmission surrounds almost every "expectant mother with hepatitis B." A Sichuan mother will take her child to have a check-up next week. She hasn't slept well for a long time. "If the check-up comes out bad, I can't talk to my husband and mother-in-law. ”
Such feelings of guilt and anxiety permeate Zhang Qingying's clinic. "The baby lives in the mother's womb for ten months," and therefore, people are more strict on women. Also carrying hepatitis B virus, in fertility, compared to women, men show a lot less trouble.
to block
Eight years ago, Zhang Qingying met a woman who was 26 weeks pregnant with cirrhosis. Her hepatitis B virus came from her mother. "In our capacity at the time, this pregnant woman risked her life by continuing her pregnancy. But this mother is very insistent, she said, 'I want this baby if I die'.
The hospital formed a team, doctors in the hepatology department and doctors in obstetrics and gynecology, "Even to the degree of cirrhosis, patients can rely on their own physical ability to get pregnant, indicating that the liver is not bad to that extent, or a glimmer of hope."
For the process of treatment, Zhang Qingying said very simple, "while walking to see," "according to her virus number to judge, see if you need to use antiviral drug treatment, how to use; After the child is born must vaccinate hepatitis B vaccine and hepatitis b immunoglobulin, this is the most important.The mother gave birth at 38 weeks and survived, with her hepatitis B virus completely blocked.
The plan, which is now very mature, was a big challenge for Zhang and her colleagues eight years ago. "At that time, I did not know how much effect there would be, and what effect it would achieve. It was slowly groping, until now it has become a guide and a consensus. Just like new crown pneumonia, the treatment process is constantly trying to find the least risk and the most effective. ”
It was under the guidance of such a plan that Gu Xia gave birth to a healthy daughter. At this point, it had been eight years since she gave birth to her first child.
Before entering her second marriage, she was completely honest about her situation. Her husband accepted her condition, consulted a doctor, was vaccinated against hepatitis B and has not been infected.
On the issue of having children, Gu Xia made a request, "Beijing's medical conditions are good, I want to give birth in Beijing. ”
She has pregnancy tests every half a month, and her mood fluctuates with the rise and fall of her hepatitis B number. "The virus count was once very high, always to the eighth power," the doctor prescribed antiviral drugs, dropped to the sixth power, the next month to the third power, and has remained there ever since.
To reduce intrauterine infection, Gu was asked to replace amniocentesis with a noninvasive prenatal test, which could obtain a "relatively accurate answer" from peripheral venous blood.
After childbirth, the midwife will immediately take the child away, quickly leave the environment contaminated by maternal blood, completely remove the child's body blood, mucus and amniotic fluid, wipe the surface of the umbilical cord will cut it.
These are not the conditions for the birth of a first child, from the pregnancy to the confirmation of her daughter's health, Gu Xia kept thinking of the first birth.
"It would have been nice to have done the same back then. "That thought popped into her head a thousand times.
After his son was diagnosed with "Little Sanyang," doctors in Beijing advised parents to cooperate with treatment with their children. "If they are not well treated in childhood, they will develop into chronic virus carriers in adulthood. ”
But the treatment was stopped after a few years by her former husband, who took the children back to his hometown in Anhui."Big expenses are the main reason, nearly one hundred thousand dollars a year. "The child is also in pain, and the interferon makes his mood bad," even banging his head against a wall. "
More important, is the vision of the people around. "Neighbors know you've gone to the doctor, and parents will tell their children not to play with him."Her ex-husband always felt that "this stigma is not brought by the disease itself, but because of the treatment."
No one spoke to his son about what had happened to him, and the boy, who had become increasingly silent, seemed accustomed to being taken in for regular checkups.
Gu Xia can only be silent, she can't even imagine, sit down and talk with her son. "'Son, it was mother who gave you the virus,' is it? It's hard just to open your mouth. ”
Let him see it first. Me too. ”
Tens of millions of "silent"
Li Bei, 27, showed something possible about the future of Gu Xia's son.
It was only after her birth that the mother was informed that both mother and daughter had contracted hepatitis B. As a minor, she shuttled regularly with her mother between the city's infectious disease hospital and home, but her mother alone remained in the doctor's office following orders.
It wasn't until the college entrance examination that she learned she was a hepatitis B virus carrier.
"Do you blame your mother? ”
"No. She's also a victim, and she doesn't want to. ”
But Libe still felt trapped. She wants to go into a love, want a marriage, but afraid to see each other's eyes mind.
Her mother advised her to hide it. "I can't. This lie must be followed by a series of lies."
It's something medicine can't solve.
In Zhang Qingying's consulting room, someone wants the doctor to erase the history of hepatitis B on the sick leave; There are husbands who wish to keep secret, not to his wife that he is infected with hepatitis B virus, and some people with her husband and doctors to play a good discussion, hidden parents-in-law.
These go far beyond the job of doctors "saving lives."
For her husband, who wants to help hide his hepatitis B, she also carefully balances privacy and health. "Telling your wife to get the vaccine in advance, telling her to make antibodies in her body, can reduce a lot of unnecessary risks. But more we will not say, do not destroy the family. ”
Zhang Qingying will also tell pregnant women who want to hide their in-laws, she can entrust a person to communicate their own situation, such as her husband, "Other people who are not within the scope of authorization, we have no right to inform, the other side has no rights to know." ”
Doctors understand the concerns of people infected with hepatitis B. The easy and effective HBV surface antigen test has singled them out from the crowd, but no one has been able to eliminate the virus completely.
From day one of diagnosis, fear was born.Public misconceptions about the infectiousness and transmission of hepatitis B place people living with the virus in the awkward position of being marginalized and may be forced to abandon their previous thoughts. Thus, silence also from this time began to become one of the protective colors of the society they live in.
Some of them, "take medicine secretly," cover their "go to infectious disease hospital," guilty to write down a "good" in the company's health condition inquiry, even voice is stressed to conceal identity.Apart from the medicine box and the checklist, everything related to "hepatitis B" was stripped from their lives, consciously or unconsciously.
Gu Xia's brother is 33 years old this year, because of the hepatitis B virus, talked about love, but did not follow, has not married. The originally cheerful and lively boy became silent.
"In our group, sometimes it is the patient to find the patient, I think my brother really can not find a like this. ”
But she dare not mention, "'Hepatitis B' is a taboo in the dialogue between siblings, a mention, brother on the flip. Shout loudly, 'What do you know?' ”
Only once, brother with her proposed, want to take nephew from her sister's ex-husband side, "The child is too poor, I come to keep good. ”
With transaminase elevated, can statins continue to use?
Sun Guolong from Ding Xiang Garden
Statins, namely hydroxymethylglutaryl CoA (HMG-CoA) reductase inhibitors, By inhibiting the synthesis of cholesterol in the body, play the role of lipid regulation, but also stable atherosclerosis plaque, anti-inflammatory, improve the stability of vascular endothelial cells and other functions, clinical widely used in coronary heart disease, stroke and other diseases of secondary prevention.
But clinically, many patients with statins have elevated transaminase in the course of treatment, and some patients even develop drug-induced hepatitis. Can statins continue to be used after liver dysfunction? How should the indications and strategies of drug modification be defined
01. What are the characteristics of statin-induced transaminase elevation?
Related data show that all statins may cause elevated transaminase. In approximately 1-2% of all patients receiving statins, elevated liver enzyme levels were more than three times the upper limit of normal.
The increase of transaminase induced by statins occurred in a dose-dependent manner within 3 months after drug initiation, and the liver enzyme level decreased after drug cessation.
At present, most scholars believe that transaminase transient beyond the normal range is the result of organ adaptation to statins and cholesterol reduction, not a sign of liver damage.
02. Elevated transaminase occurs. How to adjust medication?
1. For asymptomatic patients with simple elevated transaminase (transaminases < 3 ULN), there is no need to adjust dosage or discontinue treatment;
2. If AST and / or ALT ≥ 3 ULN during the course of administration, the drug should be stopped or reduced, and liver function should be reviewed weekly until normal;
3. Patients with elevated transaminase accompanied by large liver, jaundice, elevated direct bilirubin or prolonged coagulation time should be considered for withdrawal;
4. Patients with mildly impaired liver function with nonalcoholic fatty liver (NAFLD), hepatitis B (HBV), and hepatitis C (HCV) and compensatory cirrhosis, It is safe to use statins. Liver function monitoring should be strengthened in patients with HBV and compensated cirrhosis.
5. Statins are prohibited in patients with active liver disease, decompensated cirrhosis and acute liver failure;
6. Rosuvastatin is hydrophilic, 90% of which is excreted through the kidney in its original form. It should be used in patients with liver dysfunction.
7. Atorvastatin, simvastatin and other mainly through the liver metabolism after clearance by bile, renal dysfunction should be used.
03. Or Alternative Medicine
1. Ezekimeb
As a cholesterol absorption inhibitor, ezetimibe is the second-line drug of choice when current statin intolerance or treatment with statins alone is substandard.
In clinical controlled studies with ezetimibe alone, the incidence of elevated transaminase (ALT / AST ≥ 3 ULN) was similar to that of placebo.
For patients with mild hepatic insufficiency (Child-Pugh score 5-6), there is no need to adjust the dosage. Ezetimibe is not recommended for patients with moderate to severe liver dysfunction.
2. Bile Acid Chelators
As basic anion exchange resin, it binds with bile acid in the small intestine to prevent its reabsorption, and promotes cholesterol synthesis of bile acids in the liver, thereby increasing the activity of liver LDL-C receptor and removing LDL-c from plasma.
Common adverse reactions include gastrointestinal discomfort, constipation and affecting the absorption of certain drugs. Absolute contraindications for such drugs are complete biliary atresia, abnormal beta-lipoproteinemia, and serum TG > 4.5 mmol/L (400 mg/dL).
3. PCSK9 inhibitors
PCSK9 is a secretory serine protease synthesized by the liver, which binds to and degrades LDL receptors, thereby reducing the removal of LDL-C from serum by HDL receptors. By inhibiting PCSK9, LDL receptor degradation can be prevented and LDL-C clearance can be promoted.
The results showed that PCSK9 inhibitors, either alone or in combination with statins, significantly reduced serum LDL-C levels and improved other lipid indicators.
Preliminary clinical findings suggest that the drug reduces LDL-C by 40 to 70 percent and reduces cardiovascular events. No serious or life-threatening adverse reactions have been reported so far.
COVID-19: the turning point for gender equality
Published Online July 16, 2021 https://doi.org/10.1016/ S0140-6736(21)01651-2
The historian Walter Scheidel has argued that reductions in inequality have often emerged after war, revolution, state collapse, and plague.1 On July 12, 2021, there were more than 4 million deaths from COVID-19 globally.2 The disproportionate and unequal impact of COVID-19 on populations has brought renewed attention to deep inequalities. Will the impacts of COVID-19 galvanise efforts to reduce inequality?
One of the greatest inequalities globally is the inequity in the access to safe, effective health care without financial burden—universal health coverage (UHC). Historically, universal health reform has often been borne out of crisis. The Overseas Development Institute reported 71% of countries made progress towards UHC after episodes of “state fragility”,3 and there are plenty of examples across the continents. In 1938, after the Great Depression, New Zealand's Social Security Act began its commitment to UHC. The National Health Service in the UK was founded in 1948 in the wake of World War 2. Similarly, France and Japan enacted universal health reform after the conflict. In the aftermath of Rwanda's genocide of 1994, the country's new leadership focused on health for all and expanded UHC.4 Sri Lanka's publicly funded UHC system emerged from a devastating malaria epidemic,5 and after the 2003 SARS pandemic, China launched health-care reform to achieve universal coverage of basic health care by the end of 2020.6 In Thailand, decades of planning were realised with the launch of the Universal Coverage Scheme in 2002 after the Asian financial crisis.7 It is therefore possible that, like other crises before it, the COVID-19 pandemic could catalyse UHC reforms, should global leaders choose to harness the opportunity.8
Indeed, some countries, such as Finland and Cyprus, are implementing ambitious reforms to extend health coverage during the pandemic. In Cyprus, the second phase of their publicly financed General Health Scheme (GHS) was launched in June, 2020. These reforms are popular, attaining an 80% approval rating in a national survey.9
US President Joe Biden has a clear opportunity to expand health-care access to more people. The USA and Ireland are the only two countries in the Organisation for Economic Co-operation and Development without a universal health system. While in Ireland attempts are being made to accelerate UHC through national Sláintecare reforms,10 in the USA Biden's election stance on health care was for slow, incremental steps towards UHC.11 But now, in 2021, there is growing momentum for UHC reforms at a state level, especially in New York. Furthermore, in 2020 63% of Americans polled agreed that it is the federal government's responsibility to make sure all people have health-care coverage.12 If Biden does not harness this momentum, he could miss this unprecedented opportunity to bring UHC to the USA.
UHC is not only an option for high-income countries like the USA. Political leadership, and not a country's wealth, is a key determining factor in progress to UHC.3 Consequently, the COVID-19 crisis might provide a political window of opportunity for leaders in low-income and middle-income countries to launch UHC reforms.
South Africa is a country where some universal health reforms already came from crisis. When the African National Congress came to power in 1994, it inherited an inequitable “two-tiered” health system.13 One of the first major social policies of the then President Nelson Mandela was to launch universal free health care for pregnant women and children younger than 6 years. Yet, despite this advance, in the first decade of post-apartheid South Africa overall inequalities grew.14 After the 2019 election, the new South African Government reaffirmed its commitments to ensuring that quality health care is available to all citizens, with National Health Insurance at the centre of policy development. Although this policy enjoys considerable public support, the financing reforms needed for wealthy citizens to subsidise the rest of the population are yet to be implemented. However, there are indications that President Cyril Ramaphosa could use the COVID-19 crisis to drive through these reforms.15
COVID-19 impact on bladder cancer-orientations for diagnosing, decision making, and treatment
Thiago C Travassos, Joao Marcos Ibrahim De Oliveira, [...], and Leonardo O Reis
Introduction
The world is going through an unprecedented time in history with the arising of COVID-19. In the past, epidemics were something not as unusual as they are today, but humankind never faced a so global and widespread disease like the one caused by SARS-CoV-2.
Like many Oncology physicians, Urologists are facing and combating on two fronts: against the pandemic itself and cancer. Among all genitourinary cancers, bladder cancers are, probably, the most challenging one regarding timely decision making. Patients are usually in their late 60 s and early 70 s, more vulnerable against COVID-19, have multiple comorbidities and some will need chemotherapy.
Regarding fatality rates, bladder cancer overcomes COVID-19 by far, however, it is not the only aspect Urologist must aim at. A lot of panics have been spread in the last months, many patients are worried to be submitted to surgeries and even seeking help for health issues; and, as a consequence of it, a great percentage of them will suffer, not from the virus itself, but the consequences of it in the healthcare systems and on the psychological and dynamics of the individual and the society.
The questions are: who should be investigated and submitted to the environment of hospitals or clinics, how to investigate in the most efficient way, which patients can wait, which will need to be treated, what is the best way to treat each stage of the disease and how to proceed with these patients’ follow-up.
History has proven that pandemics have an end; but in the meantime, Urologists will have to decide which patients to expose to the health system, which ones will need more urgent intervention, and above all, to think how decisions will reflect on patients and the healthcare system in the short and long-term, with implications for years to come.
Patients with low-grade non-invasive bladder cancer have a reduced potential for disease progression when compared to patients with the muscle-invasive disease. Postponing a cystectomy surgical procedure or completing neoadjuvant chemotherapy beyond 12 weeks puts the disease’s progression and stage at risk [1].
Although follow-up cystoscopies can be performed on an outpatient basis, the risk of COVID-19 infection should not be disregarded, and the postponement of this procedure should be used to prioritize patients with a higher risk of disease progression. Regarding the previous standard follow-up, examinations of patients with non-invasive bladder cancer may be postponed, while the muscle-invasive must have a more rigorous follow-up, considering the risk-benefit of early diagnosis of relapse and thus the treatment [2].
Based on the current literature on optimal bladder cancer patients approach we comprehensively synthetize the major societies guidelines on the issue so far, adding a critical view to the topic. This article aims to guide Urologists on decision making against bladder cancer in the COVID-19 era.
The patient approach based on data analysis and risk stratification (Table 1)
Risk group stratification
One of the worst days of patients’ lives is at cancer diagnosis and it can significantly worsen if the appropriate care access is limited. That’s the dilemma Urologists have in their hands.
The global burden of bladder cancer is significantly high, representing 3.0% of all new cancer diagnoses, 2.1% of all cancer deaths in 2018 [3], and the 10th most frequently diagnosed cancer worldwide. In Europe, the incidence and mortality rates are higher in the Southern; in 2018 the age-standardized incidence and mortality rate were 15.2 per 100,000 inhabitants and the number of deaths was 64,966 [4].
Regarding the United States (US), the annual death rate from 2013 to 2017 (adjusted to the 2000 US standard population) was 4.4 per 100,000. For 2020, the American Cancer Society estimates 81,400 cases of bladder cancer, which represents 4.5% of all new cancer cases, leading to 17,980 deaths [5].
COVID-19 data changes every day. The April-26th 2020 World Health Organization (WHO) Situation Report showed a total of 2,804,796 confirmed cases, 193,722 deaths. Spain registered 219,764 cases and 22,524 deaths and the United States 899,281 cases, with 46,204 deaths [6].
In absolute death numbers, COVID-19 beats bladder cancer by far, but the analysis of the numbers can be very confusing and uncertain because of differences in adopted models used for data measuring. Even when the correct epidemiological terms are used, the number of tests and the eligibility criteria for doing it can, alone, make fatality rates vary from 0.35% in Israel to 11% in Italy at the end of March 2020. WHO Situation Report, shows a 6.9% overall case fatality rate [7].
But how to compare all of these numbers? Once diagnosed with bladder cancer the overall case fatality rate all over the world (2012) and in the United Kingdom (2015-2017) were respectively 38% and 52%, and it is estimated to be 22% in the US for 2020. The situation can be analyzed from a different perspective. COVID-19 has, indeed, killed many people; but mostly because of its great potential of spreading (infections and cases) since its fatality rate remains low. On the other hand, when someone is diagnosed with bladder cancer the chance of dying of it can be as high as 52%, so the consequences of delaying definitive treatment might impact clinical outcomes and be felt far beyond the COVID-19 outbreak, for years to come [8].
Even so, some considerations are important for shared decision making. A pandemic outbreak puts the healthcare system under extreme pressure. Many hospitals are interrupting elective surgeries to preserve health teams, ventilators, standard rooms, and Intensive Care Unit (ICU) capacity.
The American College of Surgeons advises that decisions about proceeding with elective surgeries should not be made in isolation, but use frequently shared information systems and local resources constrain, especially protective gear for providers and patients. “This will allow providers to understand the potential impact each decision may have on limiting the hospital’s capacity to respond to the pandemic. For elective cases with a high likelihood of postoperative ICU or respirator utilization, it will be more imperative that the risk of delay to the individual patient is balanced against the imminent availability of these resources for patients with COVID-19” [9].
Patients have to be aware that surgery, even during the incubation period of COVID-19, can be a risk factor for postoperative complications, ICU need, and mortality. It’s also important to look deeply into a specific age fatality rate. In China, approximately 80% of deaths occurred in people over the 60 s. In the United States 31% of cases, 45% of hospitalizations, 53% of ICU admissions, and 80% of deaths happened among people at the age of 65 or more. Using March/2020 as a parameter, while the overall case fatality rate was 3.5%, case-fatality rates varied from 2.7 to 4.9% at 65-74 to 4.3 to 10.5% at ages 75-84, showing that age plays an important role in outcomes, especially in the age range when bladder cancer is more prevalent. Patients have to know that the real scenario, an ongoing pandemic, can be vastly underestimated and that data and protocols can change day by day [7,8].
Patient selection to undergo cystoscopy
Two different situations must be distinguished: (1) Patients not yet diagnosed with bladder cancer and (2) Follow-up patients [10].
Macroscopic hematuria is per se a very challenging symptom for Urologists as it is frightening for patients. Both truths added to COVID-19 make its management even more challenging. Although no internationally accepted uniform algorithm exists, visible hematuria always requires investigation as its presence represents a risk of about 20.4% malignancy while in microscopic hematuria this risk is around 2.7%. Cystoscopy remains the diagnostic test of choice for bladder cancer and in cases of unequivocal lesions on US or urography computed tomography the indication is to proceed immediately to transurethral resection of the bladder (TURB) [11,12].
The fact is that the ideal, painless, outpatient, flexible cystoscopies are not the reality in most developing countries where the procedures (rigid cystoscopy) occur in the operation room during hospitalization, exposing the patient, even if for a brief period, to the hospital environment.
Despite that, in the presence of macroscopic hematuria the Cleveland Clinic and the American Urological Association (AUA), recommend performing full evaluation without delay, as scheduled. In the presence of microscopic hematuria with risk factors (smoking history, occupational/chemical exposure, irritate voiding symptoms), diagnostic cystoscopy can be delayed up to 3 months unless the patient is symptomatic. If there are no risk factors, evaluation can be delayed as long as necessary [13].
Regarding follow-up, the EAU divides situations into four levels of priority according to clinical harm (progression, metastasis, loss of renal function) risk. (1) Low: very unlikely if postponed 6 months; (2) Intermediate: possible if postponed 3-4 months, but unlikely; (3) High: clinical harm and cancer-related death very likely if postponed for more than 6 weeks; (4) Emergency: a life-threatening situation or opioid-dependent pain, treated at emergency departments despite current pandemic [14].
The recommended for low priority bladder cancer, patients with low or intermediate-risk non-muscle-invasive bladder cancer (NMIBC) without hematuria, is to defer cystoscopy by 6 months. Intermediate priority patients, with a history of high-risk NMIBC without hematuria, might be followed up before the end of 3 months. High priority patients, with NMIBC and intermittent hematuria, must undergo follow-up cystoscopy in a period inferior to 6 weeks. In case of emergencies (visible hematuria with clots, urinary retention) cystoscopy or TURB must be considered within less than 24 hours (Table 2). EAU guideline is the only one to specify the level of confidence of its recommendations (all the above-cited, level 3) [14].
Cystoscopy follow-up
AUA guideline recommends considering surveillance cystoscopy without delay for assessment of response to treatment or surveillance of high-risk NMIBC within 6 months of initial diagnosis. For high-risk NMIBC beyond 6 months of initial diagnosis, the recommendation is to consider delaying evaluation for up to 3 months. Assessment of response to treatment or surveillance of low/intermediate-risk NMIBC regardless of when the diagnosis was made may be delayed for 3 to 6 months [13].
Considerations regarding computed tomography and hematuria
All over the world, SARS-CoV-2 is putting healthcare systems under a lot of pressure, and computed tomography (CT) is being used for diagnosis, management, and follow-up of COVID-19. Although CTs, using specific urological protocols, is the gold-standard method for the investigation of most urological pathologies, this new scenario is forcing Urologists to review and adapt.
The DETECT I (Detecting Bladder Cancer Using the UroMark Test), a prospective, observational, multicentric study showed that patients with microscopic hematuria had 2.7%, 0.4%, and 0% incidence of bladder cancer, renal and upper tract urothelial cancer, respectively, and that the approach with cystoscopy and renal and bladder ultrasound (RBUS), instead of CT could be used, in cases of microscopic hematuria. On the other hand, RBUS accuracy alone to detect bladder cancer was poor with 63.6% sensitivity, reinforcing that for bladder cancer diagnosis, cystoscopy remains the gold standard and CT urography continues to be the upper tract investigation method of choice [15].
In concern to follow-up, EAU guideline is the only one that provides some guidance and recommends to defer by 6 months upper tract imaging in patients with a history of high-risk NMIBC (low priority) [14].
Therapeutical and surgical indications for patients with bladder cancer in the COVID era
AUA is following the guidance of the American College of Surgeons which devised surgeons to look at the Elective Surgery Acuity Scale (ESAS) from the St Louis University for decision making during the COVID-19 outbreak. This scale is graduated from tier 1 to 3, with subdivisions (a) and (b). Most cancers are classified as 3a (high acuity surgery/health patient) which must not be postponed. There is no specific mention regarding bladder cancer patients [16]. The Cleveland Clinic Department of Urology is more specific regarding procedures as it stratifies patients from 0 (emergency) to 4 (nonessential) and specifies surgeries; although its tables and text are very poor at explaining acronyms. In this guideline cystectomies (high-risk CA) and TURB (high-risk) are stratified as 1 (0-4) while TURB low risk, as 4 [13].
EAU guideline uses the same method for cystoscopy, strafing patients in priority categories (low, intermediate, high, and emergency) and is more specific and complete [14]. We will summarize all recommendations, dividing the disease in its classic risk stratification, using, mainly, EAU guideline, because of its consistency. It is not the scope of this article to discourse about the TNM staging system and it will be used as in EAU guideline. Also, important to say that most of the statements were directly extracted from the guideline but rearranged, in a more didactic way.
Non-muscle-invasive bladder cancer
According to EAU guideline [14] TURB can be delayed by 6 months in patients with small papillary recurrence/s (less than 1 cm) and a history of Ta/1 low-grade tumors. If feasible maybe just followed or fulgurated during office cystoscopy. The second TURB in patients with visibly complete initial TURB of T1 lesion with muscle in the specimen can also be deferred by 6 months. In these cases, TURB also can be postponed after Bacillus Calmette-Guérin (BCG) intravesical instillations.
Patients with any primary tumor or recurrent papillary tumor greater than 1 cm and without hematuria or history of high-risk NMIBC must be treated before the end of 3 months. In cases with bladder lesions and intermittent macroscopic hematuria or a history of high-risk NMIBC, TURB must be done within less than 6 weeks. All patients confirmed or suspected of bladder cancer presenting macroscopic hematuria with clot retention or/and requiring bladder catheterization ought to be treated in a time inferior to 24 hours. Any patient with the highest-risk NMIBC must be considered for immediate radical cystectomy.
Muscle invasive bladder cancer
According to EAU guideline [14] In cases when Muscle Invasive Bladder Cancer (MIBC) is diagnosed, staging imaging by CT thorax-abdomen-pelvis should not be delayed. On the other hand, in cases when images are suspicious for invasive tumors, TURB must be performed. In both cases, CT or TURB must be done in 6 weeks.
The proven benefit of neoadjuvant chemotherapy (NAC) in T2 tumors, is limited and has to be weighed against the risks, especially in patients with a short life expectancy and those with (pulmonary and cardiac) comorbidity. The same is valid for focal T3 N0M0 tumors. That cisplatin eligible, high burden T3/T4 N0M0, NAC risk should be individualized while they are on the waiting list, but treatment should be offered before 6 weeks. All inclusion in chemotherapy trials must be delayed, except for cisplatin eligible patients.
Regarding radical cystectomy (RC), it can be offered for patients with T2-T4a, N0M0 tumors and must be performed before the end of 3 months. Once RC is scheduled the urinary diversion or organ-preserving techniques should be done as would be planed outside this crisis period. Multimodality bladder sparing therapy can be considered for selected T2N0M0 patients [17]. In cases where palliative cystectomy is considered as intractable hematuria with anemia, alternatives such as radiotherapy (RT), with or without chemotherapy, must be discussed. In the presence of anemia, it is important to start treatment in less than 24 hours, other palliative cases may wait not more than 6 weeks.
Adjuvant cisplatin-based chemotherapy can be offered to those patients with pT3/4 and/or pN+ disease if no NAC has been given and must be started in less than 6 weeks.
Metastatic bladder cancer
Oncologists play a central role to advise the feasibility of non-surgical treatments like radiotherapy or chemotherapy in the management of malignancy mainly in these uncertain times the world is facing [17]. In the words of Dr. Thomas Powles, Professor of Genitourinary Oncology and Director of the Barts Cancer Centre in London, “(…) if you’re going to give chemotherapy today (…) Don’t think about what it looks like today. Think what might it look like in two weeks before you push the patient into that swimming pool, not knowing how long they’re going to be under the water for” [18].
The key point is to assess risk and benefit individually in each patient. In asymptomatic patients with low disease burden, the first-line therapy can, in selected cases, be postponed to 8-12 weeks under clinical surveillance. EAU guideline recommends the use of cisplatin-containing combination chemotherapy with GC (gemcitabine plus cisplatin), MVAC (methotrexate, vinblastine, adriamycin plus cisplatin), preferably with G-CSF (granulocyte colony-stimulating factor), HD-MVAC (high dose-MVAC) with G-CSF or PCG (paclitaxel, cisplatin, gemcitabine). In this period (inferior to 3 months) offer checkpoint inhibitors pembrolizumab or atezolizumab depending on PD-L1 (programmed death-ligand 1) status [14].
In symptomatic metastatic patients, the benefit of treatment is likely higher than the risk and these patients should initiate treatment within less than 6 weeks. Supportive measures such as the use of GCSF should be considered. The recommendations are the same for the asymptomatic patients being treated. As second-line therapy, checkpoint inhibitor pembrolizumab can the offered to patients progressing during, or after, platinum-based combination chemotherapy for metastatic disease. Alternatively, offering treatment within a clinical trial setting can be an option [14].
Supportive care
The EAU guideline recommends that acute renal failure, for locally advanced bladder cancer, must be treated with nephrostomy at ambulatory settings [14]; not a reality for most developing countries in the world, where nephrostomies are done in the operating rooms with improvised materials. Embolization or hemostatic RT ought to be considered for bleeding with hemodynamic repercussion.
Considerations regarding BCG and intravesical instillations (Table 3)
BCG and intravesical instillations
There is no evidence that patients receiving intravesical BCG have a higher risk of COVID-19 and the recommendation for not initiating, stopping, or postponing are mainly because the risk of contracting the virus when going to a health care facility might overcome the risk of delaying doses for some time.
EAU guidelines orientate to abandon early postoperative instillation of chemotherapy in presumably low or intermediate-risk tumors as in confirmed intermediate-risk NMIBC. In high-risk NMIBC the recommendation is to initiate treatment within less than 6 weeks with intravesical BCG immunotherapy with one-year maintenance [15]. AUA guideline recommends that, for intermediate and high-risk NMIBC, induction BCG should be prioritized, once induction provides a significant benefit by reducing disease recurrence and progression; though they may also require a delay in therapy depending on local needs and resources. On the other hand, maintenance intravesical BCG should be stopped and reevaluated in 3 months for high-risk and delayed indefinitely in intermediate-risk because the most significant impact of the intravesical treatment is obtained during the induction course [13].
Does BCG immunotherapy impact COVID-19? A study including 40 individuals that received the trivalent influenza vaccine, 14 days after randomly (20 × 20) being injected with BCG or placebo shows potential [19]; there is a therapeutic (https://clinicaltrials.gov/ct2/show/NCT04369794) and some preventive trials underway studying the effect of BCG vaccination on increasing resistance to infection and preventing severe COVID-19 infection. Also, regarding intravesical BCG potential cross-protection against COVID-19, considering its T cell boosting mechanisms, we are starting the “Global Inquire of Intravesical BCG As Not Tumor but COVID-19 Solution” - “GIANTS” trial.
Considerations regarding surgical procedures
Viral RNA has been detected in feces from day 5 up to 4-5 weeks after symptoms in moderate cases. Wang et al., investigated the biodistribution of SARS-CoV-2 in different tissues, collecting 1,070 specimens from 205 patients with COVID-19. Of the feces samples, 29% tested positive compared to only 1% (3 of 307) blood samples, and none of the 72 urine samples, confirmed by another recent study where the virus was not detectable in the urine of tested patients [20,21]. These data have clear implications for surgeons when considering radical cystectomy and make TURB a more comfortable environment. Whenever possible, Urologist should test their patients for SARS-CoV-2 48 hours before surgery, not a very feasible reality in most developing countries.
Regarding laparoscopic surgery, many considerations can be done and full discussion of it is far beyond the objective of this article, even though some are worth discussing. Despite no conclusive evidence regarding the difference in risks of viral transmission, of open and laparoscopic surgery for the surgical team, the last one can be associated with a higher amount of smoke particles in the operation room. Recommended modifications are to keep intraperitoneal pressure as low as possible, to aspirate the inflated CO2 before removing the trocars, and to lower electrocautery power settings. Laparoscopic procedures, due to the lack of evidence for not performing it during the COVID-19 outbreak, must be considered as any minimally invasive procedure, that might be associated with shorter length of hospital stay, use of resources, and personal [22].
For robotic surgeries, the same cautions must be taken with some particularities, as avoiding using two-way pneumoperitoneum insufflators to prevent pathogens colonization of circulating aerosol in the pneumoperitoneum circuit or the insufflator. These integrated flow systems need to be configured in a continuous smoke evacuation and filtration mode. Aerosol dispersal is even more important when concerning robotic surgeries because of the common need of a not exchangeable operating room where the mobile cart, the image cart, and the console are at more risk of contamination due to particles in the air [23].
Conclusions
When comparing diseases and their epidemiological impacts, the mortality rates are a very common thermometer to help healthcare administrators and physicians on decision making, but when facing a novel disease as COVID-19, there has not been enough time to evaluate the damage regarding mortality. When looking at the fatality rates, bladder cancer overcomes COVID-19 by far and can be as high as 52%, so Urologists must not postpone investigation. Cystoscopy remains the gold standard for the investigation of bladder cancer and CT urography for obtaining images of the upper tract in cases of macroscopic hematuria. The use of ultrasound is reserved for imaging the upper tract in cases of microscopic hematuria. EAU guideline provides the most specific orientations in cases of bladder cancer and they are summarized above. Whenever TURB is necessary, extra care must be taken to assure muscle sample, avoiding another surgical intervention and hospitalization, but when necessary it should not be postponed due to the elevated progression rate of the disease. With this study, we can propose a new way to perform the screening and monitoring of bladder cancer, considering the aggressiveness and the capacity to progress depending on its stage. Follow-up cystoscopies can be postponed for 6 months for low risk, 3 months for intermediate, 6 weeks for high risk, and no longer than 24 hours in case of emergencies such as life-threatening hematuria, anemia, and urinary retention. This innovation in monitoring can bring greater safety to the patient, especially in those at higher risk, prioritizing and preventing the progression of the disease and guaranteeing their agile treatment when necessary, since the centers will have more time to schedule cystoscopies during pandemics. Regarding chemotherapy, more than ever the key point is to evaluate each case individually. BCG must be considered only as an inducing course, in selected intermediate and most high-risk cancers; all others should be stopped. Whenever possible patients should be tested before surgery.
Research involving human participants: The authors certify that the study was performed under the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Developing a New Medicine or Device
secondscount.org
There are five basic stages of development that a novel treatment must pass through before approval. Many good ideas for novel treatments don't even make it through these stages due to a variety of factors such as incomplete paperwork or lack of funding. A collaboration involving researchers, doctors, regulators and the private company that owns the patent on the medication or device determine how the trials are set up. Although clinical trials for device approval typically require enrolling fewer patients than do drug trials, this gap has been narrowing as device trials are subject to increasingly rigorous scientific standards.
The Five Stages of Development
The five key stages of clinical trials that a novel device or medication must pass through before - and after - it reaches the market include:
Preclinical
The safety and effectiveness of experimental medications or devices are evaluated in test tubes, computer models and often on animals. For medicines, this involves assessing how the compounds move through living organisms and what impact they have against the disease target. Likewise, devices also must be evaluated for how compatible they are with the human body and how they work within the body.
The main goal of preclinical studies is to rigorously assess safety before human tests begin; this is why preclinical studies often take three to six years (or longer) to conduct. Some preclinical safety tests continue even after the start of clinical trials to help identify any long-term adverse effects. Once ready for the next stage of testing on humans, the researcher or scientist must file an investigational medicine or device application with the U.S. Food and Drug Administration (FDA) before human testing may begin. The application must show:
Results of preclinical experiments
The chemical structure of the compound or design of the device
How it is thought to work in the body
Any side effects found in animal studies; and
How it will be manufactured.
The application must also include a detailed plan of how, where, and by whom the clinical trial will be conducted.
In addition, all clinical trials must be approved and monitored by an Institutional Review Board (IRB), a committee that reviews biomedical and behavioral research involving humans. An IRB is typically set up by academic institutions and medical facilities, but they can also be created by for-profit companies and are called independent or commercial IRBs. The aim of the IRB is to protect the rights and welfare of those involved in the study. Progress reports on clinical trials must be submitted at least annually to IRBs and the FDA.
Pilot, or Phase 1
Researchers first test an experimental medication or device in a small group of people to evaluate its safety, determine a safe dosage range and identify side effects. To establish the safety profile of an experimental medication and determine how it moves through the body, a pilot study may involve 20 to 100 healthy volunteers. Somewhat fewer participants (a dozen or more) are needed for devices. This process can take from six months to a year to complete.
Feasibility, or Phase 2
The experimental medication or device is given to a larger group of patients who have the disease or condition to test whether it is effective and further evaluate its safety. For medications, these trials can involve 100 to 500 participants. Typically the group is divided in two, with one half given a placebo (an inactive substance, often called a "sugar pill"), and the other given the "active" medication. The placebo group is referred to as the control group.
In device trials, rather than implant an inactive device, the control group typically receives the standard treatment for the disease or condition. The goal of this phase is to prove whether the therapy effectively treats the disease. Researchers continue to evaluate the safety of the medication or device, look for side effects and adjust the therapy (such as dosage level). These studies also typically take from six months to a year.
Pivotal, or Phase 3
The pivotal stage is the phase of clinical trials designed to evaluate safety and effectiveness (efficacy) on a wide sampling of participants - from hundreds to 5,000 or more - of the target patient group. For medications, these are large, randomized (that is, the participants are randomly assigned to one of two or more treatment "arms," or groups), placebo-controlled trials that generate statistically significant data. This means the results are unlikely to have been reached by chance or coincidence.
Researchers closely and regularly monitor patients to confirm effectiveness and identify adverse events or side effects. They compare the safety and effectiveness of the new therapy to treatments already in common use for the targeted disease or condition. These studies can take from one to four years to complete, depending on the design of the study and how long it takes to recruit enough patients to meet the minimum size requirements established for the trial.
After Phase 3
Once the three phases of the clinical trials are complete, the data are analyzed to determine if the experimental medication or device is safe and effective. If it is, a new medication or device application is filed with the FDA.
FDA scientists review the study results and determine whether the medication or device is safe and effective enough to be "cleared for marketing." In some cases, an Advisory Committee composed of FDA-appointed experts is convened to review the application and recommend whether it should be approved and, if so, under what conditions. The FDA is not required to accept an Advisory Committee's recommendations, but it typically does accept them.
It took an average of 16.9 months for the FDA to review each medicine it approved in 2003. The proportion of applications rejected at this point in the approval process has remained constant over the years at about 10-15 percent.
Off-Label Use of Drugs & Devices
Once cleared for marketing, the medication or device is available to physicians and patients. In the United States, FDA regulations permit doctors and other health care providers to prescribe approved medications and devices for indications other than the disease or condition for which they are approved; this is called off-label use. Learn more about off-label use here.
Post-marketing, or Phase 4
Patients participating in the clinical trial are followed for a year or more - sometimes many years - after a medication or device receives regulatory approval to monitor for safety and effectiveness and to gather additional information about risks, benefits, and optimal use. Since a much bigger and more diverse group of patients is now likely to take the medicine or have the device, researchers may detect side effects or adverse events that were not apparent during clinical trials. This is why researchers must submit regular reports to the FDA detailing complications they observe. These studies also help researchers better assess how the medication or device affects a particular group of patients based on such criteria as age, sex, race or condition.
Types of Studies
Studies are conducted using varying methods and are commonly classified as observational or interventional. Common study classifications include:
Observational studies meaning that researchers only observe study participants and do not intervene in their care or treatment program. These studies are not considered clinical trials.
Observational retrospective cohort studies collect past data and information from the medical records of two groups of similar human populations who differ in only one key characteristic, to measure a specific outcome. An example of this would be looking for the prevalence of lung cancer in a population of 40-year-old Caucasian women where half of the population smokes tobacco and half do not smoke at all.
Prospective cohort studies follow a similar human population over a certain time period where the population has key differentiating factors with respect to the study. Researchers observe these differentiations to determine how they affect the study's outcome.
Registry studies observe and collect clinical data about the effectiveness and use of a medication or medical device in a human population that has already received the medication or device. These studies are typically broad and do not exclude participants based on age, gender, race, etc.
Case control studies compare a population with a certain medical condition to a very similar population without the medical condition, to determine factors that may lead to the condition.
Interventional studies mean that researchers give study participants a particular medicine or medical device to assess the outcome. Most clinical trials are classified as interventional studies.
First-in-man studies are when a medication or device that has previously been tested on a non-living organism or animal is tested on humans for the first time.
Cost-Effectiveness of Hypertension Treatment by Pharmacists in Black Barbershops(Abstract)
Kelsey B. Bryant, MD, MPH, MS Andrew E. Moran, MD, MPH Dhruv S. Kazi, MD, MSc Yiyi Zhang, PhD Joanne Penko, MS, MPH Natalia Ruiz-Negrón, PharmD Pamela Coxson, PhD Ciantel A. Blyler, PharmD Kathleen Lynch, PharmD Laura P. Cohen, MD, MPP Gabriel S. Tajeu, DrPH, MPH Valy Fontil, MD, MAS Norma B. Moy, BA Joseph E. Ebinger, MD, MS Florian Rader, MD Kirsten Bibbins-Domingo, PhD, MD Brandon K. BellowsPharmD, MS
Originally published15 Apr 2021https://doi.org/10.1161/CIRCULATIONAHA.120.051683Circulation. 2021;143:2384–2394
Background:
In LABBPS (Los Angeles Barbershop Blood Pressure Study), pharmacist-led hypertension care in Los Angeles County Black-owned barbershops significantly improved blood pressure control in non-Hispanic Black men with uncontrolled hypertension at baseline. In this analysis, 10-year health outcomes and health care costs of 1 year of the LABBPS intervention versus control are projected.
Methods:
A discrete event simulation of hypertension care processes projected blood pressure, medication-related adverse events, fatal and nonfatal cardiovascular disease events, and noncardiovascular disease death in LABBPS participants. Program costs, total direct health care costs (2019 US dollars), and quality-adjusted life-years (QALYs) were estimated for the LABBPS intervention and control arms from a health care sector perspective over a 10-year horizon. Future costs and QALYs were discounted 3% annually. High and intermediate cost-effectiveness thresholds were defined as <$50 000 and <$150 000 per QALY gained, respectively.
Results:
At 10 years, the intervention was projected to cost an average of $2356 (95% uncertainty interval, –$264 to $4611) more per participant than the control arm and gain 0.06 (95% uncertainty interval, 0.01–0.10) QALYs. The LABBPS intervention was highly cost-effective, with a mean cost of $42 717 per QALY gained (58% probability of being highly and 96% of being at least intermediately cost-effective). Exclusive use of generic drugs improved the cost-effectiveness to $17 162 per QALY gained. The LABBPS intervention would be only intermediately cost-effective if pharmacists were less likely to intensify antihypertensive medications when systolic blood pressure was ≥150 mm Hg or if pharmacist weekly time driving to barbershops increased.
Conclusions:
Hypertension care delivered by clinical pharmacists in Black barbershops is a highly cost-effective way to improve blood pressure control in Black men.